How does echocardiography detect coronary artery disease?
Echocardiography, particularly stress echocardiography, can be used to detect coronary artery disease (CAD), although it does not visualize the coronary arteries directly like angiography. Instead, it assesses the heart’s function and structure, which can be affected by CAD. Here’s how it works:
- Wall Motion Abnormalities: CAD can lead to areas of the heart muscle receiving insufficient blood supply (ischemia), especially under stress. Echocardiography can detect abnormal motion of the heart’s walls, which might indicate areas where blood flow is compromised due to blockages in the coronary arteries.
- Rest and Stress Echocardiography: A standard echocardiogram provides images of the heart at rest. However, in stress echocardiography, images are also taken after the heart is stressed, either through exercise or medication. This stress can reveal problems with blood flow that are not apparent when the heart is at rest.
- Changes in Ejection Fraction: The ejection fraction (EF) is the percentage of blood that is pumped out of the ventricles with each heartbeat. CAD can decrease the EF, especially during exercise, which can be observed in a stress echocardiogram.
- Doppler Echocardiography: This technique assesses blood flow within the heart and can indicate problems related to CAD, such as reduced flow velocity or turbulent flow in the heart’s chambers, which might suggest underlying ischemia.
- Diastolic Dysfunction: CAD can affect the heart’s ability to relax properly between beats (diastolic function). Echocardiography can detect signs of diastolic dysfunction, which might be related to coronary artery disease.
- Secondary Signs: Echocardiography might also reveal secondary signs of CAD, such as thickening of the heart muscle (hypertrophy), which can develop over time due to chronic ischemia.
It’s important to note that while echocardiography can provide valuable information about the heart’s function and indirect clues about the presence of CAD, it is not typically used as the sole diagnostic tool for CAD. Other tests, like coronary angiography, CT angiography, or nuclear stress tests, are more direct in assessing the coronary arteries themselves. Echocardiography is often used as part of a comprehensive assessment, especially in evaluating heart function and the effects of known or suspected CAD on the heart.
How does echocardiography detect Heart Failure?
Echocardiography is a crucial tool in the diagnosis and management of heart failure. It helps in assessing the structure and function of the heart, which can be significantly affected in heart failure. Here’s how echocardiography detects heart failure:
- Ejection Fraction (EF) Assessment: Echocardiography measures the ejection fraction, which is the percentage of blood the left ventricle pumps out with each contraction. In heart failure with reduced ejection fraction (HFrEF), the EF is usually below normal, indicating a weakened heart muscle.
- Wall Motion and Thickness: The test can reveal abnormalities in the movement and thickness of the heart’s walls. In heart failure, these walls may be abnormally thickened (hypertrophy) or weakened and dilated.
- Heart Size and Chamber Volumes: Heart failure often leads to enlargement of the heart chambers, especially the left ventricle. Echocardiography can measure these chamber sizes and volumes, providing important information about the severity and type of heart failure.
- Diastolic Function: Echocardiography evaluates diastolic function, or how well the heart relaxes and fills with blood. In heart failure with preserved ejection fraction (HFpEF), the heart’s ability to relax and fill may be impaired, even though the ejection fraction remains normal.
- Valvular Function: Heart failure can be caused or worsened by problems with the heart valves. Echocardiography can assess the function of these valves, detecting any stenosis (narrowing) or regurgitation (leakage) that could contribute to heart failure.
- Assessment of the Pericardium: The test also evaluates the pericardium (the sac surrounding the heart). Conditions like constrictive pericarditis can mimic heart failure and can be identified on an echocardiogram.
- Hemodynamic Information: Doppler echocardiography provides information on blood flow within the heart, which can help in assessing the hemodynamic status of a patient with heart failure.
- Determining the Cause: Echocardiography can help in identifying the underlying cause of heart failure, such as coronary artery disease, hypertension, cardiomyopathies, or congenital heart disease.
By providing detailed images and information about the heart’s structure and function, echocardiography is essential in confirming the diagnosis of heart failure, determining its severity and type, guiding treatment decisions, and monitoring the disease’s progression and response to treatment.
Ideally who all should get an echocardiography done?
Echocardiography is a valuable diagnostic tool in cardiology, but it’s not routinely performed on everyone. Ideally, the following groups of people should consider getting an echocardiography:
- Symptomatic Individuals: Those experiencing symptoms suggestive of heart problems, such as chest pain, shortness of breath, palpitations, fainting spells (syncope), or fatigue, should undergo an echocardiogram.
- History of Heart Disease: Individuals with a known history of heart conditions, including coronary artery disease, heart valve disease, cardiomyopathy, or congenital heart defects, often need regular echocardiograms to monitor their condition.
- High Risk for Heart Disease: People with risk factors such as hypertension, diabetes, high cholesterol, obesity, a family history of heart disease, or a history of smoking may benefit from echocardiography, especially if they have symptoms or other clinical findings suggestive of heart disease.
- Before and After Heart Surgery: Echocardiography is commonly used to evaluate the heart’s function and structure before and after heart surgery, including valve repair or replacement, and coronary artery bypass grafting.
- Abnormal Clinical Findings: Those with abnormal findings on a physical examination, such as a heart murmur, irregular heartbeat, or signs of heart failure, should have an echocardiogram.
- Monitoring Certain Medical Treatments: Patients undergoing treatments that can affect the heart, such as chemotherapy or radiation therapy to the chest, may require periodic echocardiograms.
- Infection-related Heart Issues: Individuals with conditions such as endocarditis (infection of the heart lining) or pericarditis (infection of the covering of the heart) should undergo echocardiography for diagnostic purposes.
- Athletes with Suspected Heart Problems: Athletes, especially those in competitive sports, who have symptoms or a family history of sudden cardiac death, may undergo echocardiography as part of their screening process.
It’s important to remember that the decision to perform an echocardiogram should be based on individual clinical circumstances and is typically made by a healthcare provider. The test is used as a diagnostic tool when there is a suspicion or risk of heart disease, rather than as a routine screening test in the general population without symptoms or significant risk factors.
I am a 45 year old woman, weighing around 75 Kg, Height 165 Cm., with Diabetes and Hypertension of 12 years standing. I am not having any symptoms of Heart Disease. Recently I came across a mention of a new syndrome called HFpEF in social media, alerting all over-weight women, particulary Diabetics, to get assessed. Is it correct?
The condition you’re referring to, HFpEF (Heart Failure with preserved Ejection Fraction), is indeed a recognized cardiac syndrome, and your concerns are valid given your medical profile. Here’s some insight into HFpEF and whether you should consider getting assessed:
- What is HFpEF?: HFpEF occurs when the left ventricle of the heart is unable to fill properly during the diastolic phase (when the heart relaxes and fills with blood). This leads to symptoms of heart failure despite a normal ejection fraction (a measure of how well the heart pumps blood).
- Risk Factors: The risk factors for HFpEF include hypertension, diabetes, obesity, and age. Being a 45-year-old woman with a history of diabetes and hypertension, you fall into a higher risk category for this condition.
- Symptoms of HFpEF: Common symptoms include shortness of breath, fatigue, and swelling in the legs and abdomen. However, HFpEF can sometimes be asymptomatic or its symptoms might be attributed to other conditions, which makes diagnosis challenging.
- Importance of Assessment: For individuals with risk factors like yours, it can be prudent to undergo periodic cardiac assessments, even in the absence of overt heart disease symptoms. These assessments might include echocardiography, which is key in diagnosing HFpEF.
- Lifestyle and Management: For those at risk of HFpEF, managing risk factors through lifestyle changes, like diet and exercise, and controlling hypertension and diabetes is crucial.
- Consulting a Healthcare Provider: It’s essential to discuss with your healthcare provider about the need for cardiac assessment. They can evaluate your individual risk and decide if tests like an echocardiogram are necessary.
- Awareness and Proactivity: The mention you came across on social media highlights the importance of being proactive about heart health, especially in populations at risk like overweight diabetic women.
While social media can provide useful health information, it’s always best to seek advice from healthcare professionals who can provide personalized recommendations based on your health history and current condition. In your case, considering an evaluation for HFpEF could be a wise step, but this decision should be made in consultation with your doctor.
What is a GLPS data in detecting and managing Heart Failure?
The term “GLPS” in the context of heart failure likely refers to “Global Longitudinal Peak Strain,” which is a parameter measured in cardiac imaging, particularly in speckle tracking echocardiography (STE). Here’s an overview of what it is and its role in detecting and managing heart failure:
- What is Global Longitudinal Peak Strain (GLPS)?
- GLPS is a measure of the deformation (strain) of the heart muscle during each heartbeat. Specifically, it assesses how much the length of the heart muscle fibers shortens (contracts) in the longitudinal direction (from the base to the apex of the heart) during a cardiac cycle.
- This measure is expressed as a percentage. A higher negative value (e.g., -20%) indicates better function, whereas lower negative values (e.g., -10%) suggest impaired myocardial deformation.
- Detection of Heart Failure:
- In heart failure, especially Heart Failure with Preserved Ejection Fraction (HFpEF), traditional measures like Ejection Fraction (EF) can be normal, making diagnosis challenging.
- GLPS offers a more sensitive measure of left ventricular systolic function than EF. It can detect subtle changes in the heart’s pumping ability, often identifying dysfunction before EF decreases.
- This makes GLPS particularly valuable in the early detection of heart failure when other measures might still be within normal ranges.
- Management of Heart Failure:
- Monitoring GLPS over time can help in assessing the progression of heart failure and the response to treatment. Changes in GLPS can indicate improvements or worsening of cardiac function, guiding therapeutic decisions.
- In patients with established heart failure, regular assessment of GLPS can aid in optimizing medical therapy and timing interventions.
- Prognostic Value:
- Studies have shown that GLPS has prognostic value in various cardiac conditions, including heart failure. Abnormal GLPS values can predict adverse outcomes and help in risk stratification of patients.
- Technological Advancement:
- The use of STE for measuring GLPS represents an advancement in cardiac imaging, providing more detailed and accurate assessments of cardiac mechanics compared to traditional echocardiography.
In summary, GLPS is a sophisticated echocardiographic measure that provides detailed insights into the heart’s pumping efficiency, particularly useful in the early detection, management, and risk assessment of heart failure. It’s especially important in cases where other indicators like EF are not showing significant abnormalities.
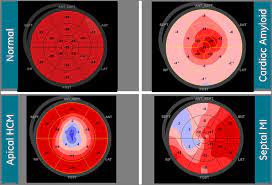
Why should I insist on a “bulleye” every time an echocardiogram is taken?
The term “bullseye” in the context of heart failure refers to “Global Longitudinal Peak Strain,” which is a parameter measured in cardiac imaging, particularly in speckle tracking echocardiography (STE). Here’s an overview of what it is and its role in detecting and managing heart failure:
- What is a bullseye?
- The Americaln Heart Association (AHA) and the Europian Society of Cardiology (ESC) recognize the pumping chamber (Left Ventricle) to be comprised of 17 segments. Each segment has to perform optimally, in order to get a good ejection of blood from the heart. Every time the cardiac fibers contract (deformation), the heart pump is able to perform to its best. This deformation (in negative numbers) is color coded and presented as a bullseye, and the values of deformation are given as negative numbers. From these figures and pictures, one is able to get a comprehensive view about the heart’s function.
- Detection of Heart Failure:
- In heart failure, especially Heart Failure with Preserved Ejection Fraction (HFpEF), traditional measures like Ejection Fraction (EF) can be normal, making diagnosis challenging.
- Bullseye offers a more sensitive measure of left ventricular systolic function than Ejection Fraction (EF). It can detect subtle changes in the heart’s pumping ability, often identifying dysfunction before EF decreases.
- This makes GLPS particularly valuable in the early detection of heart failure when other measures might still be within normal ranges.
- Management of Heart Failure:
- Monitoring bullseye over time can help in assessing the progression of heart failure and the response to treatment. Changes in Bullseye pattern can indicate improvements or worsening of cardiac function, guiding therapeutic decisions.
- In patients with established heart failure, regular assessment of GLPS can aid in optimizing medical therapy and timing interventions.
- Prognostic Value:
- Studies have shown that the bullseye has prognostic value in various cardiac conditions, including heart failure. Abnormal Bullseye can predict adverse outcomes and help in risk stratification of patients.
- Technological Advancement:
- The use of STE for measuring GLPS represents an advancement in cardiac imaging, providing more detailed and accurate assessments of cardiac mechanics compared to traditional echocardiography.
In summary, the bullseye is a sophisticated echocardiographic measure that provides detailed insights into the heart’s pumping efficiency, particularly useful in the early detection, management, and risk assessment of heart failure. It’s especially important in cases where other indicators like EF are not showing significant abnormalities.