Excerpt
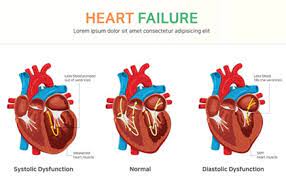
Heart failure, a global health issue, occurs when the heart can’t pump blood efficiently, leading to decreased oxygen and nutrient supply to organs. It’s more than a singular condition; it’s a spectrum of disorders affecting the heart’s blood supply ability. Systolic heart failure (Heart Failure with Reduced Ejection Fraction (HFrEF), a common type, happens when the heart muscle’s contraction ability is compromised, resulting in insufficient blood pumping. It’s now termed , characterized by a low ejection fraction measured through echocardiography. Diastolic heart failure, an equally important type of Heart Failure with Preserved Ejection Fraction (HFpEF), occurs as a result of difficulty of the pumping chamber to relax. Symptoms like fatigue, breathlessness, and reduced exercise capacity are linked to heart failure of both types. Diagnosis involves clinical evaluation and tests like echocardiograms, highlighting the underlying pathology in the heart.
Introduction
The Heart is the Capital of Mind —
The Mind is a single State —
The Heart and the Mind together make A single Continent.
-Emily Dickinson’s “The Heart”
Heart failure is a major health issue around the world. It happens when the heart can’t pump blood well enough, leading to a decrease in the supply of oxygen and nutrients to the body’s organs.
In simpler terms, it means the heart isn’t strong enough to meet the body’s needs for energy and oxygen. This is also known as “the inability to meet the metabolic demands of the tissues”.
Heart Failure is not a singular condition
Types of Heart Failure
Heart failure is not a singular condition but a spectrum of disorders affecting the heart’s ability to supply the body with sufficient blood.
Each type – systolic and diastolic – has its unique characteristics and requires specific management strategies.
Systolic Heart Failure
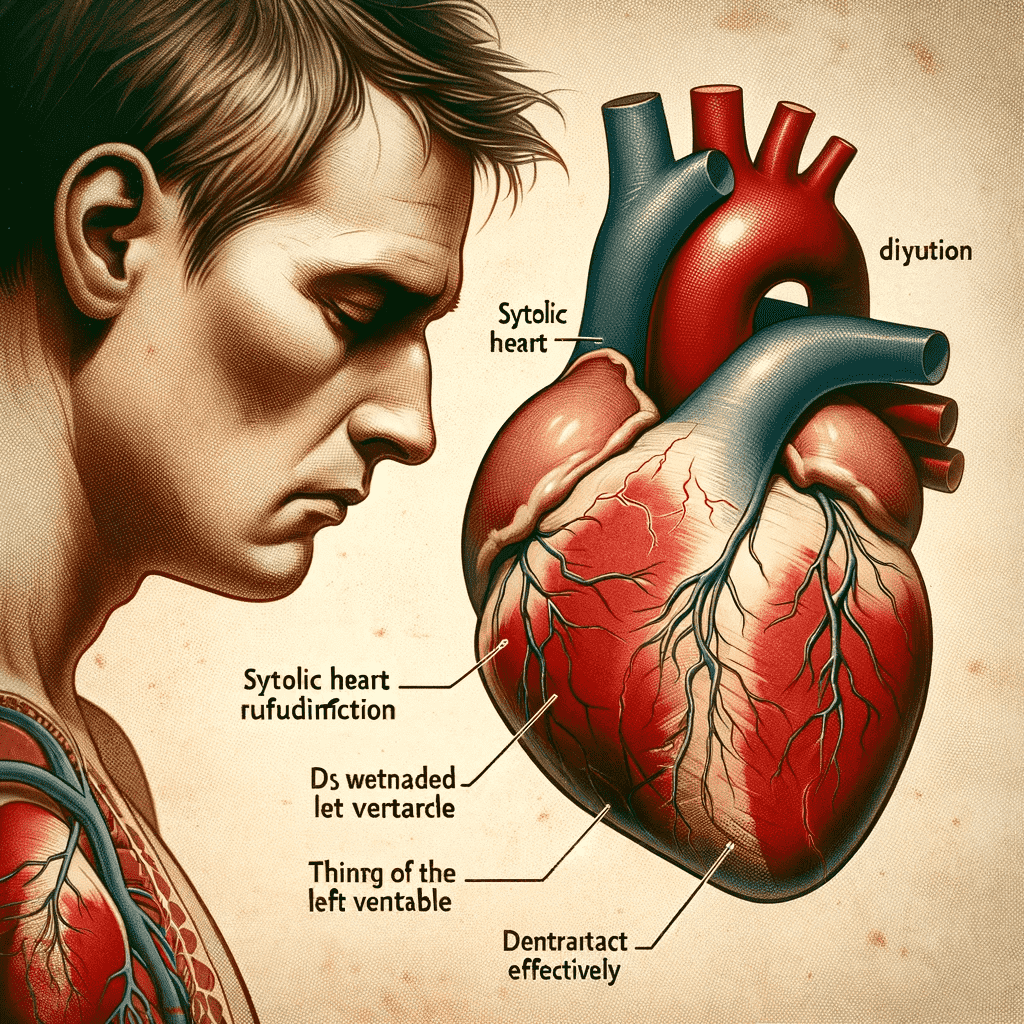
Systolic heart failure, a prevalent form of heart disease, arises when the heart muscle’s ability to contract is compromised.
This condition leads to a critical health issue: the heart’s decreased capacity to pump sufficient blood throughout the body.
Understanding systolic heart failure involves examining its definition and causes, the symptoms it presents, and the methods used for its diagnosis.
Definition and Causes of Systolic Heart Failure
The primary characteristic of systolic heart failure is the heart’s inability to contract forcefully enough during each heartbeat.
This weakened contraction means that the heart cannot pump blood efficiently, leading to a reduced output of blood to the body’s organs and tissues.
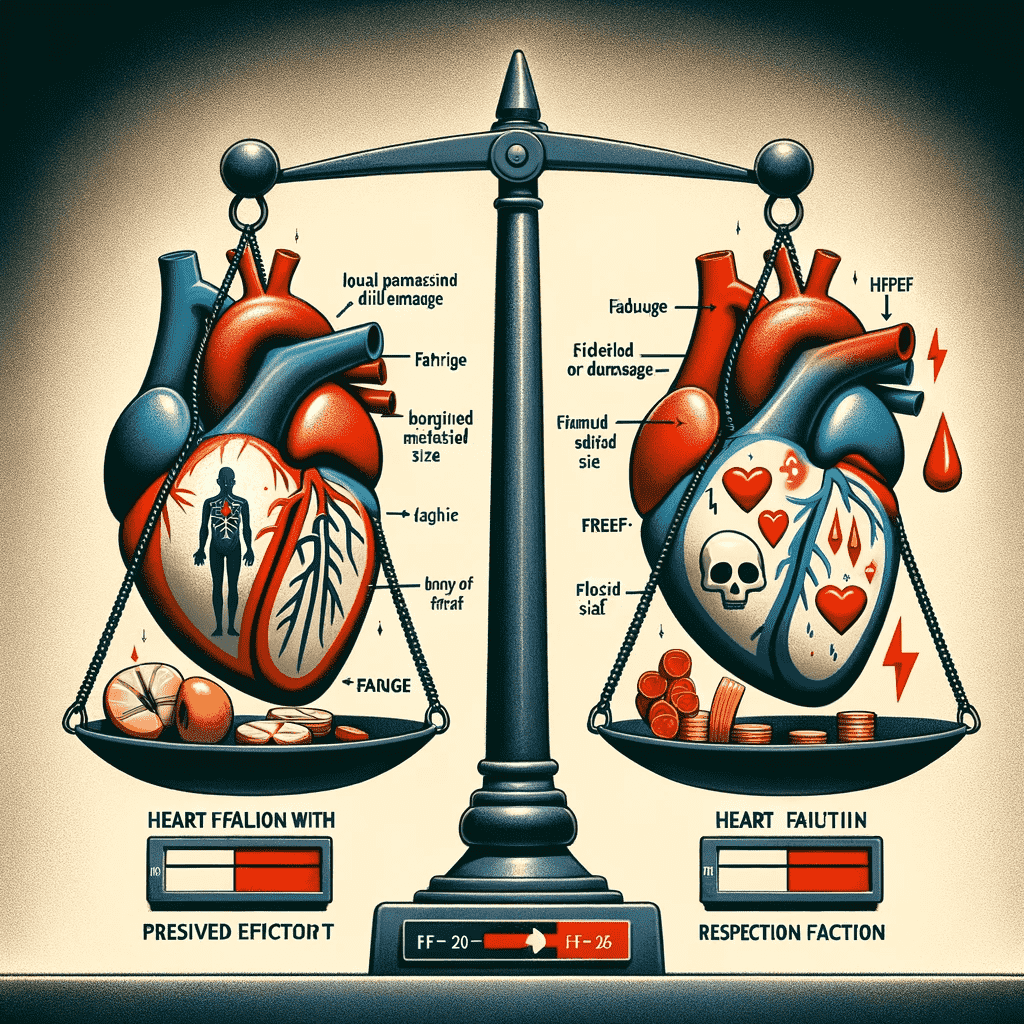
Systolic Heart Failure and HFrEF. Are they synonymous?
Systolic Heart Failure is now-a-days known as Heart Failure with Reduced Ejection Fraction (HFrEF).
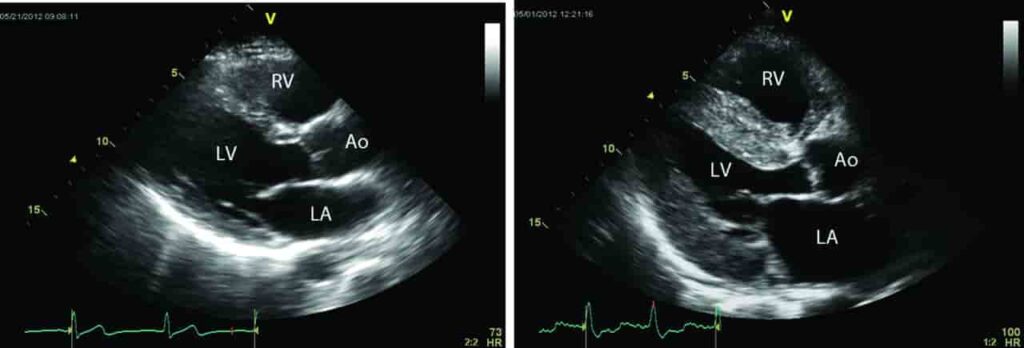
The definition is based on an Echocardiographic assessment of the pumping chamber’s efficiency, as determined by a parameter called “Left Ventricular Ejection Fraction” (LVEF or simply EF), which assesses the percentage of blood volume ejected out of the pumping chamber (LV) in comparison with the volume of blood held in its cavity during the previous holding period, called “diastole”.
What are the causes of Systolic Heart Failure (HFrEF)?
The causes of systolic heart failure are diverse, but they often trace back to any condition that can damage the heart muscle. The most common culprits include coronary artery disease (CAD) and previous heart attacks.
CAD, characterized by the narrowing of the arteries that supply blood to the heart muscle, can diminish the heart’s blood supply, weakening the muscle over time.
A heart attack, resulting from a sudden blockage in these arteries, can cause direct damage to the heart’s muscle fibers, significantly impairing their ability to contract.
Other factors contributing to systolic heart failure include conditions like hypertension, which overworks the heart, and diseases such as cardiomyopathy, which directly affect the heart muscle’s strength and elasticity.
Additionally, lifestyle factors like smoking, obesity, and a sedentary lifestyle can increase the risk of developing systolic heart failure.
What are the symptoms of Systolic Heart Failure (HFrEF)?
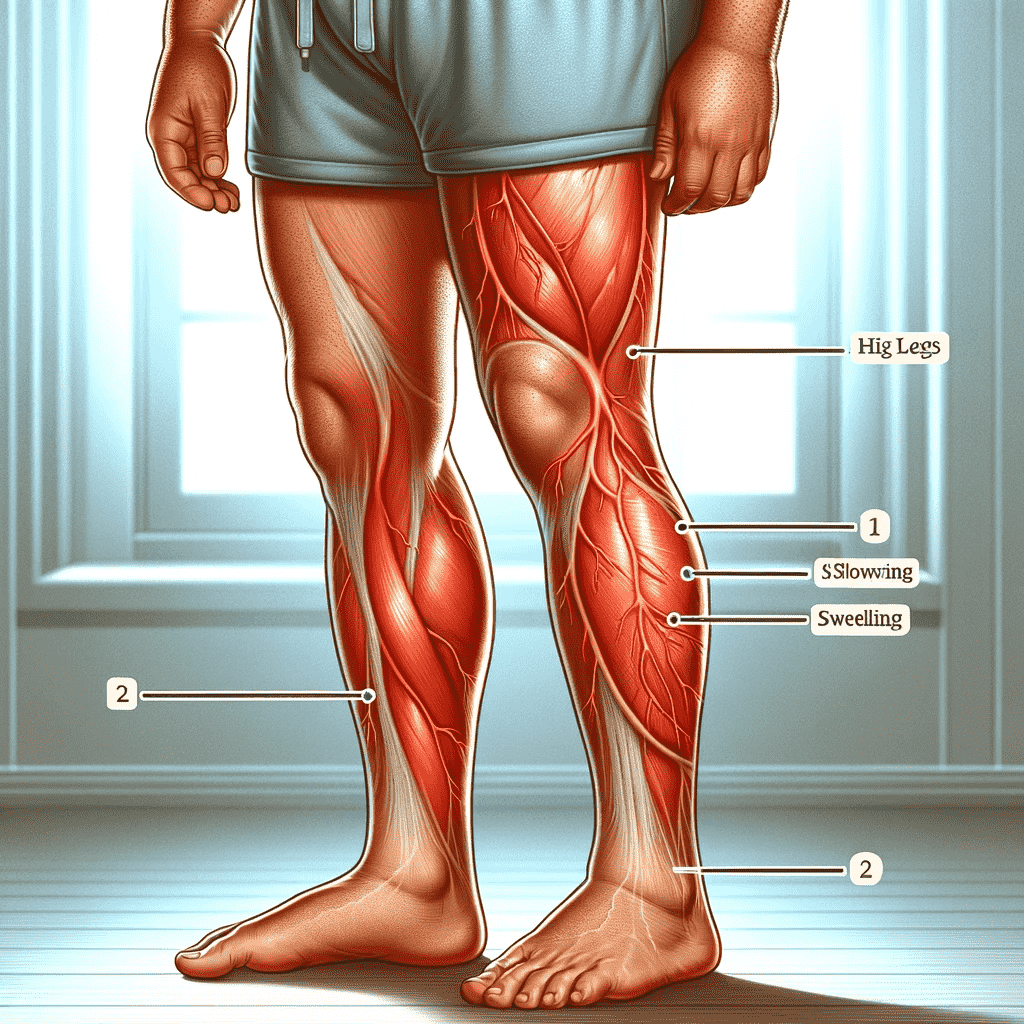
The symptoms of systolic heart failure are primarily linked to the heart’s reduced ability to pump blood.
Patients often report experiencing significant fatigue, which is attributed to the body’s organs and muscles not receiving enough oxygen-rich blood.

Breathlessness or dyspnea is another hallmark symptom, particularly noticeable during physical activities or even at rest in advanced stages. This occurs as the lungs struggle to meet the body’s oxygen demands due to the heart’s inefficiency.
A reduced exercise capacity is also commonly observed. Patients may find that activities they could perform easily before now leave them tired or short of breath.
Additionally, as the condition progresses, other symptoms such as swelling in the legs and abdomen, irregular heartbeat, and persistent cough or wheezing might develop due to fluid accumulation and the heart’s inability to keep up with the body’s demands.
How does a doctor diagnose a Systolic Heart Failure (HFrEF) ?
Diagnosing systolic heart failure involves a combination of clinical evaluation and diagnostic testing. The key metric used in the diagnosis is the ejection fraction – a measurement that indicates the percentage of blood leaving the heart each time it contracts.
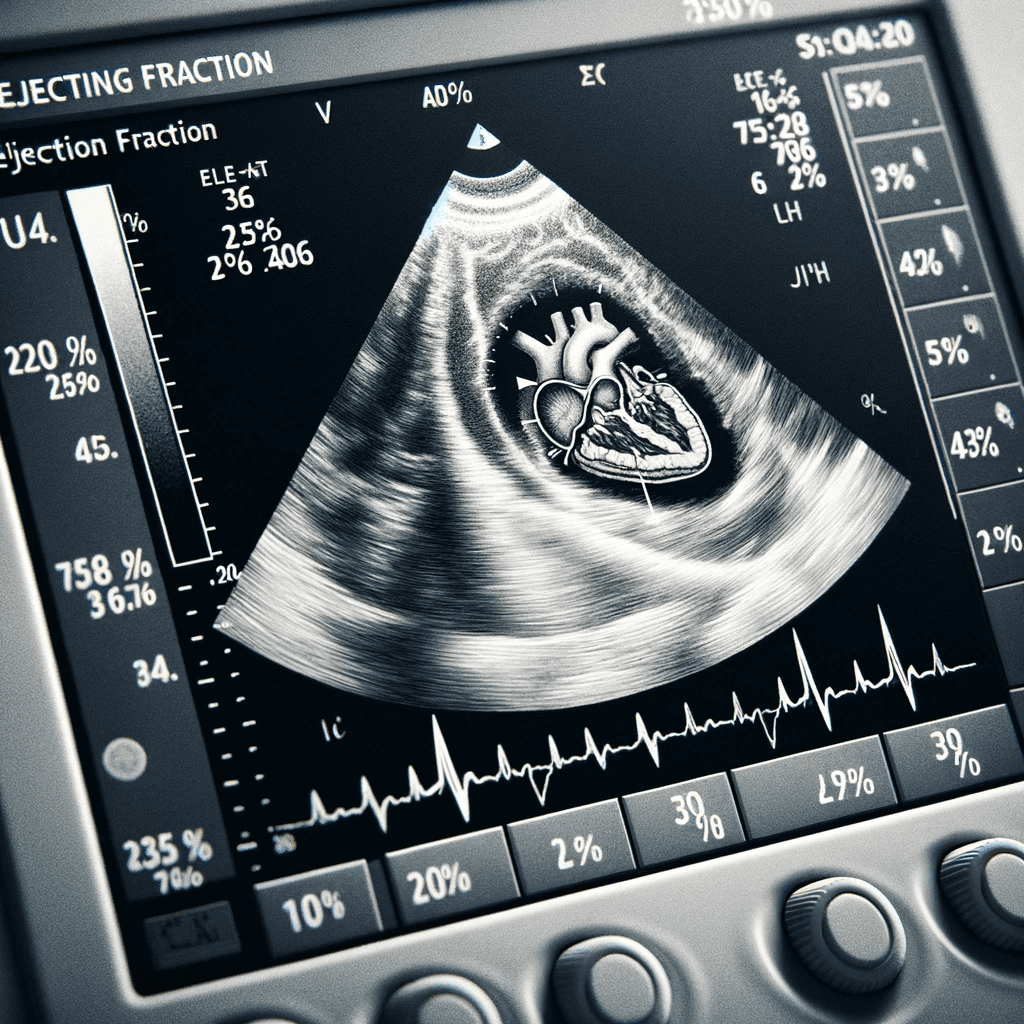
In a healthy heart, the ejection fraction is typically between 55% and 70%. In systolic heart failure, this number is significantly lower, as the heart’s weakened contractions fail to eject an adequate amount of blood.
The ejection fraction is measured using an echocardiogram, a type of ultrasound for the heart. This test provides detailed images of the heart’s structure and functioning, allowing physicians to assess the movement of the heart’s walls and the volume of blood pumped with each heartbeat.
Additionally, other tests such as electrocardiograms (ECG), chest X-rays, and blood tests for markers of heart stress and failure (like BNP or NT-proBNP) may be employed to provide a comprehensive assessment of the heart’s condition and to rule out other potential causes of the symptoms.
Therefore, systolic heart failure is a serious condition characterized by the heart’s diminished ability to contract and effectively pump blood.
Understanding its causes, recognizing its symptoms, and employing appropriate diagnostic tools are crucial steps in managing this condition. Early diagnosis and treatment are essential in improving the quality of life for those affected and in preventing the progression of the disease.
Diastolic Heart Failure
Diastolic heart failure is a significant medical condition that arises from the stiffening of the heart muscle, impeding its ability to fill with blood effectively. Its symptoms, though similar to systolic heart failure, often require a keen clinical eye to differentiate and accurately diagnose.
Understanding this type of heart failure is vital, as it necessitates a tailored approach to management and treatment, differing significantly from the strategies used in systolic heart failure. With the aging global population and the rise in conditions like hypertension and diabetes, the prevalence of diastolic heart failure is expected to increase, making awareness and understanding of this condition more important than ever.
This type of heart failure, though less discussed than its counterpart, systolic heart failure, is equally significant and poses unique challenges in terms of diagnosis and management.
Definition of Diastolic Heart Failure
Diastolic heart failure is marked by the heart’s inability to relax and expand fully during its diastolic phase – the period when the heart fills with blood. This failure in relaxation results in the heart being less effective in accommodating a sufficient volume of blood, leading to a decrease in the amount of blood pumped to the body with each heartbeat.
The primary cause of diastolic heart failure is a stiffening of the heart muscle. This stiffness can be attributed to several underlying health conditions. Hypertension (high blood pressure) is one of the most common culprits. Persistent hypertension puts extra strain on the heart, leading over time to a thickening and stiffening of the heart muscle. Diabetes is another significant risk factor; the high blood sugar levels associated with diabetes can damage the heart muscle, reducing its elasticity.
Other contributing factors include age-related changes to the heart, obesity, and certain types of heart disease, like hypertrophic cardiomyopathy. In these scenarios, the heart muscle undergoes structural changes that impede its ability to relax properly.
Symptoms of Diastolic Heart Failure
The symptoms of diastolic heart failure can be similar to those experienced in systolic heart failure but often differ in their intensity and presentation.
Shortness of Breath
The most common symptom is shortness of breath, or dyspnea, which occurs because the heart isn’t filling adequately, leading to congestion in the lungs. This symptom is particularly noticeable during physical activity or when lying flat.
Fatigue
Fatigue is another frequent symptom, resulting from the body’s organs not receiving enough oxygen-rich blood.
Rapid or Irregular Heartbeat
Patients with heart failure often experience palpitations or a feeling of a rapid, fluttering, or pounding heart. This is due to the heart’s attempt to compensate for its reduced ability to pump blood. In some cases, heart failure can lead to irregular heart rhythms (arrhythmias), which can be life-threatening.

Nausea
Nausea or a lack of appetite can also be associated with heart failure. This is often a result of congestion in the gastrointestinal tract, a consequence of fluid retention. Additionally, a bloated feeling, constipation, and abdominal discomfort can also occur.
Sudden Weight Gain Due to Fluid Retention
Unexpected weight gain is a key indicator of fluid retention in heart failure patients. This can happen rapidly, over a few days. It’s essential for patients to monitor their weight regularly, as a sudden increase could indicate worsening heart failure.
Other possible symptoms include swelling in the legs and abdomen, rapid or irregular heartbeats, and difficulty in exercising.
One key aspect of diastolic heart failure is that these symptoms can fluctuate in intensity, often worsening with physical exertion or stress.
Diagnosis of Diastolic Heart Failure
Diagnosing diastolic heart failure presents unique challenges. Unlike systolic heart failure, where the ejection fraction (a measurement of the percentage of blood leaving the heart each time it contracts) is reduced, in diastolic heart failure, the ejection fraction is often normal or near normal.
This is because the issue lies not in the heart’s ability to contract, but in its ability to relax and fill.

Therefore, the diagnosis of diastolic heart failure relies heavily on other diagnostic criteria. An echocardiogram is crucial in this regard. This imaging test not only visualizes the heart’s structure but also assesses its function during the diastolic phase.
Specific findings, such as the thickness of the heart walls and the speed of blood flow into the heart during relaxation, provide vital clues.
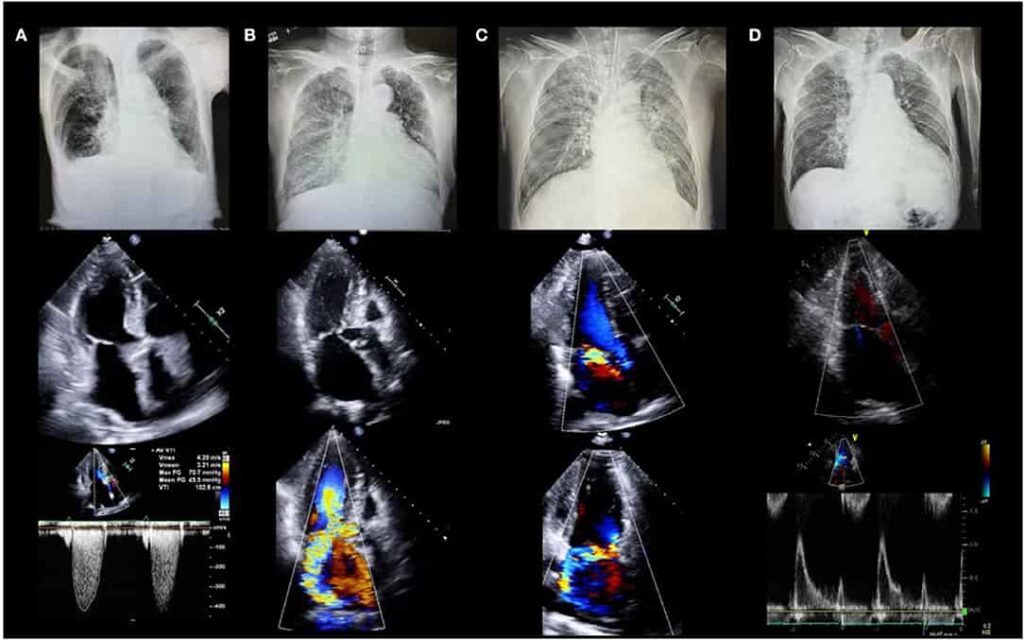
In addition to echocardiograms, other tests such as electrocardiograms (ECG), blood tests for cardiac biomarkers, and chest X-rays are used to assess heart function and rule out other conditions that might mimic the symptoms of heart failure.
Heart failure, regardless of whether it is of the systolic or diastolic type, presents a range of symptoms that are common to both forms. These symptoms are critical for the early identification and effective management of the condition.
Contact your Healthcare Professional
These common symptoms of heart failure, regardless of its type, underscore the importance of prompt diagnosis and management. Recognizing these symptoms early can lead to better treatment outcomes. It is crucial for individuals experiencing these symptoms to seek medical attention, as heart failure is a progressive condition that can worsen if left untreated. Regular monitoring, lifestyle modifications, and adherence to treatment plans can significantly improve the quality of life for those living with heart failure.

Diagnosis of Heart Failure Diagnosing heart failure involves a detailed medical history, physical examination, blood tests, imaging studies like chest X-rays and echocardiograms, and electrocardiograms (ECG). These tests help in identifying the type of heart failure and its severity.
Challenges in Heart Failure Management
Treatment strategies for heart failure are multifaceted and depend significantly on the specific type of heart failure a patient is experiencing. However, there are general approaches that are widely applicable, primarily involving lifestyle modifications, medication management, and occasionally, surgical interventions.
Lifestyle changes are a cornerstone in the management of heart failure. These changes aim at reducing the burden on the heart and improving overall cardiovascular health.
Dietary modifications are crucial; they typically include reducing salt intake to lower blood pressure and fluid retention, limiting fluid intake to avoid overload, and eating a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins. Increased physical activity is also recommended but needs to be balanced with the individual’s capacity and the severity of their heart failure.

It’s about finding the right level of exercise that benefits the heart without overstraining it. Additionally, smoking cessation is imperative as smoking is a major risk factor for heart disease and can worsen heart failure.
Medication management is tailored to each patient’s specific condition and symptoms. Commonly prescribed medications include diuretics, which help reduce fluid buildup in the body; ACE inhibitors, which lower blood pressure and reduce strain on the heart; beta-blockers, which slow the heart rate and lower blood pressure; and other medications like angiotensin II receptor blockers, aldosterone antagonists, ARNI group of drugs (Read more…) and digitalis. These medications, also known as the 4-pillars of HF management, work together to alleviate symptoms, improve heart function, and slow the progression of heart failure. (Read more…)

In some cases, when medication and lifestyle changes are not sufficient, surgical interventions may be considered. These can range from procedures to repair or replace a damaged heart valve, implantation of devices like pacemakers or defibrillators to help control heart rhythms, or in severe cases, heart transplantation.
The approach to treating heart failure is comprehensive and requires regular monitoring and adjustments by healthcare professionals, ensuring that treatment remains effective and responsive to the patient’s evolving condition (Read more…).
Collaboration between the patient and healthcare team is crucial in managing heart failure effectively.
Living with Heart Failure
Living with heart failure is a journey that involves meticulous management and adaptation to a new lifestyle. This chronic condition demands constant vigilance and a comprehensive approach to treatment and self-care. Heart failure patients must engage in regular monitoring of their weight and symptoms, as sudden changes can indicate worsening of their condition.

Weight gain, for instance, might suggest fluid retention, a common problem in heart failure. Similarly, monitoring symptoms like increased shortness of breath, fatigue, or swelling in the extremities can help in early detection of potential complications.
Dietary and fluid restrictions are pivotal in managing heart failure. Salt and fluid intake often need to be limited to prevent fluid overload, which can exacerbate heart failure symptoms and lead to hospitalization.
A diet rich in fruits, vegetables, whole grains, and lean proteins, and low in saturated fats, trans fat, and cholesterol, is recommended. Patients are often advised to avoid or limit alcohol and caffeine intake as well. These dietary changes not only help manage heart failure but also contribute to overall cardiovascular health.
Engaging in prescribed physical activity is another crucial aspect. Exercise, tailored to the individual’s capacity and the severity of their condition, can strengthen the heart and improve circulation. However, it’s important that these activities are conducted under medical supervision to avoid overexertion.

Avoiding harmful habits like smoking is non-negotiable. Smoking can accelerate the progression of heart failure by increasing the heart’s workload and damaging blood vessels. Patients are strongly advised to quit smoking and avoid exposure to secondhand smoke.
Regular follow-ups with healthcare providers are essential. These check-ups allow for adjustments in treatment, monitoring of the disease’s progression, and management of any side effects of medication. It’s a collaborative effort where the healthcare team might include cardiologists, primary care physicians, dietitians, and physical therapists. These professionals provide guidance, support, and education, helping patients navigate the complexities of heart failure.
Living with heart failure also involves emotional and mental health considerations. The chronic nature of the disease can be overwhelming, leading to feelings of anxiety and depression. Support from family, friends, and possibly professional counselors is important.
Prevention and Risk Factors
Preventing heart failure is a proactive and crucial aspect of maintaining cardiovascular health. Understanding and managing risk factors play a central role in this endeavor. Several key risk factors can significantly increase the likelihood of developing heart failure, and addressing them early can help reduce the risk.
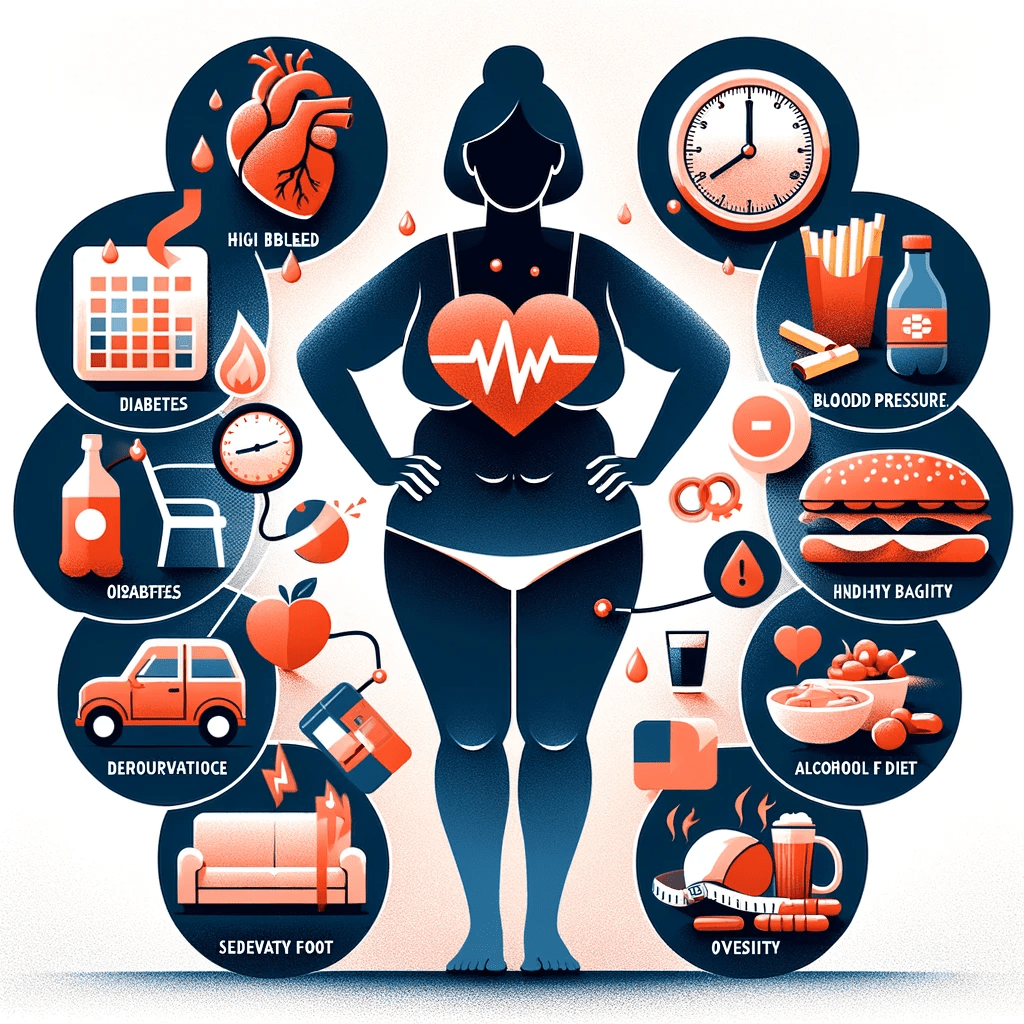
High blood pressure, or hypertension, is a major risk factor for heart failure. Managing blood pressure through lifestyle changes and medication when necessary is essential. Regular monitoring and compliance with prescribed treatments can prevent the strain on the heart that high blood pressure can cause.
Diabetes is another critical risk factor. Individuals with diabetes have an elevated risk of heart failure, making it crucial to control blood sugar levels through diet, medication, and insulin therapy as recommended by healthcare providers.
Obesity is associated with an increased risk of heart failure, as excess body weight can strain the heart. Maintaining a healthy weight through a balanced diet and regular exercise can help prevent obesity-related heart issues.
Smoking is a well-known risk factor for heart disease, including heart failure. Quitting smoking and avoiding exposure to secondhand smoke are vital steps in reducing this risk.
Regular exercise and a heart-healthy diet are fundamental components of prevention. Engaging in physical activity helps maintain cardiovascular fitness and reduces the risk of obesity, high blood pressure, and diabetes. A diet rich in fruits, vegetables, whole grains, lean proteins, and low in saturated fats and cholesterol supports heart health.

Routine health check-ups with a healthcare provider are essential for early detection and prevention. These check-ups allow for the monitoring of blood pressure, blood sugar levels, and overall cardiovascular health. Early identification of risk factors and timely interventions can prevent heart failure and promote a healthier, longer life.
Therefore, preventing heart failure involves proactive measures that focus on managing risk factors like high blood pressure, diabetes, obesity, and smoking. A heart-healthy lifestyle encompassing regular exercise, a balanced diet, and routine health check-ups is the foundation for reducing the risk of heart failure and promoting overall cardiovascular well-being.
Conclusion
In conclusion, heart failure is a complex and chronic cardiovascular condition that demands a comprehensive approach to management and prevention.
Living with heart failure requires diligent self-care, including regular monitoring of weight and symptoms, adherence to dietary and fluid restrictions, prescribed physical activity, and the cessation of harmful habits like smoking.
Collaborative efforts between patients and their healthcare teams are paramount in optimizing heart failure management.
Preventing heart failure involves recognizing and addressing risk factors such as high blood pressure, diabetes, obesity, and smoking.
Lifestyle modifications, including regular exercise and a heart-healthy diet, play a pivotal role in reducing these risks. Routine health check-ups enable early detection and intervention.
By proactively managing heart failure and addressing risk factors, individuals can enhance their quality of life and reduce the likelihood of disease progression.
Heart failure is a condition that necessitates ongoing dedication to self-care and a strong partnership with healthcare providers to ensure the best possible outcomes for those affected.