Getting to Know Enhanced External Counterpulsation (EECP)
Imagine your heart as a busy city with roads (arteries) that transport goods (blood) to various parts. Sometimes, these roads can get blocked or congested, causing traffic jams and slowing down the flow of goods. Similarly, when our heart’s arteries face challenges, blood flow can be affected. This is where Enhanced External Counterpulsation, commonly referred to as EECP, comes into play.
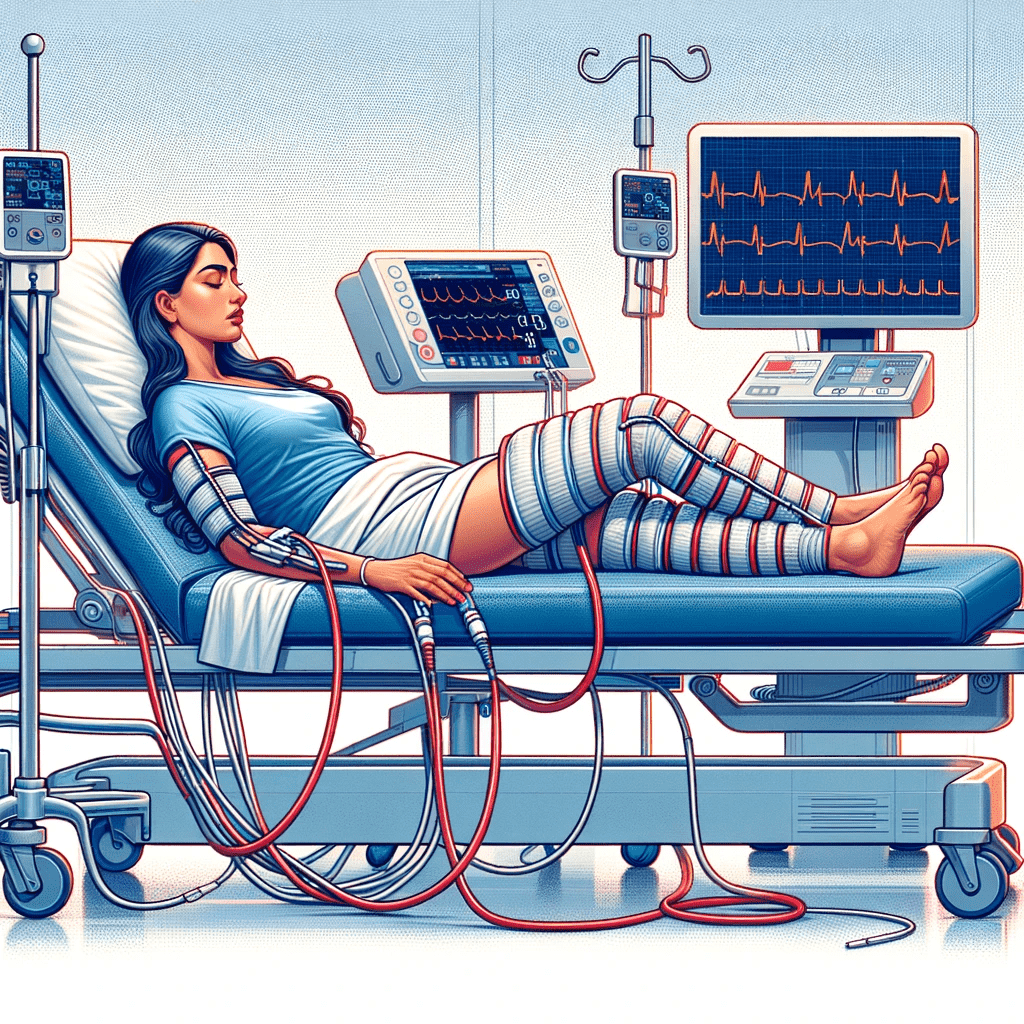
- EECP is a non-invasive treatment – meaning it doesn’t involve surgeries or any procedures inside the body. Instead, patients lie on a bed, and large blood pressure-like cuffs wrap around their legs.
- These cuffs inflate and deflate in rhythm with the patient’s heartbeat. Think of it as giving the heart a gentle push. When the heart is resting between beats, EECP helps push more blood towards it.
- This increases the blood flow and oxygen supply, which can help relieve chest pain and improve heart function.
FAQs
Why is that EECP called Natural Bypass?
Enhanced External Counterpulsation (EECP) is often referred to as a “Natural Bypass” because of its ability to promote the development of new pathways for blood flow around blocked arteries in the heart, mimicking the effects of a surgical bypass but in a non-invasive manner. Here’s why EECP is associated with this term:
- Formation of Collateral Circulation: EECP can stimulate the opening and formation of small blood vessels in the heart, known as collateral vessels. These vessels can create natural bypasses around narrowed or blocked arteries, improving blood flow to heart muscle that is otherwise compromised.
- Non-Invasive Procedure: Unlike surgical bypass, which involves major surgery to graft arteries or veins from other parts of the body to bypass blocked coronary arteries, EECP is non-surgical. It uses external cuffs on the legs to enhance blood flow.
- Enhancing Blood Flow: During EECP, cuffs on the legs inflate and deflate in sync with the heart’s rhythm. This process increases blood flow back to the heart, particularly when the heart is relaxed, and decreases the heart’s workload.
- Mimicking the Effects of Bypass Surgery: By improving blood flow to the heart muscle, EECP mimics some of the benefits of coronary artery bypass graft (CABG) surgery. However, it’s important to note that EECP is not a replacement for bypass surgery in severe cases.
- Therapeutic Angiogenesis: The improved blood flow and decreased workload on the heart can promote angiogenesis, the formation of new blood vessels. This process is akin to creating natural bypass routes in the heart.
- Symptom Relief: EECP is primarily used for the treatment of angina (chest pain due to reduced blood flow to the heart muscles). It can relieve symptoms of heart disease, similar to how bypass surgery alleviates angina.
- Used for Patients Who Cannot Undergo Surgery: EECP is often a treatment option for patients who are not candidates for bypass surgery or angioplasty due to various medical reasons.
It’s important to note that while EECP is an effective treatment for certain heart conditions, particularly for symptom relief in chronic stable angina, it is not a substitute for coronary artery bypass grafting in cases where surgical intervention is necessary. EECP is often used when traditional treatments like surgery or medication are not viable or have not been fully effective. As with any medical treatment, the suitability of EECP for a patient should be evaluated by a healthcare professional.
Should I get hospitalized for EECP?
Enhanced External Counterpulsation (EECP) treatment typically does not require hospitalization. EECP is an outpatient procedure, meaning it’s performed in a setting where you can go home after each session. Here’s how the process usually works:
- Daily Sessions: EECP treatment involves regular sessions, often scheduled daily. Each session typically lasts about one hour and is usually conducted in a specialized clinic or outpatient department of a hospital.
- Series of Treatments: The full course of EECP treatment typically includes a series of sessions, commonly ranging from 35 to 40 sessions, spread over about 7 to 8 weeks.
- During the Session: During each session, you’ll lie on a bed, and large blood pressure-like cuffs will be wrapped around your legs and buttocks. These cuffs inflate and deflate in sync with your heartbeats, which enhances blood flow to your heart.
- Return Home Afterward: After each session, you can return to your home. There’s no need for an overnight stay in the hospital.
- Continuation of Normal Activities: Outside of your treatment sessions, you can typically continue with your regular daily activities, though your doctor might provide specific advice based on your individual health condition.
- Monitoring and Evaluation: Throughout the treatment course, your healthcare provider will monitor your progress and response to the treatment. This ensures that the therapy is effectively addressing your symptoms and any underlying conditions.
- Follow-Up Care: After completing the EECP treatment course, there will be follow-up evaluations to assess the long-term benefits and any need for additional treatment or lifestyle adjustments.
Since EECP is a non-invasive procedure and does not require recovery time like surgical treatments, it’s a convenient option for many patients who qualify for it. However, always consult with your healthcare provider for personalized advice and to understand how EECP fits into your overall treatment plan.
Why is that EECP is considered the first option if I have Coronary Artery Disease or Heart Failure, rather than Interventional procedures like Balloon Angioplasy, Stenting, Bypass surgery?
Enhanced External Counterpulsation (EECP) might be considered as a first-line treatment option for Coronary Artery Disease (CAD) or Heart Failure in certain circumstances, but this decision is highly individualized and depends on the specific details of each patient’s condition. Here’s why EECP might be preferred over more invasive interventional procedures like balloon angioplasty, stenting, or bypass surgery in some cases:
- Non-Invasiveness: EECP is a non-invasive procedure, which makes it a safer option, especially for patients who have high risks associated with surgical procedures. It doesn’t require anesthesia or incisions, reducing the risk of complications like bleeding or infection.
- Patient’s Overall Health and Suitability for Surgery: Patients with multiple comorbidities, advanced age, or other factors that make them high-risk candidates for surgery might benefit from EECP as a safer alternative.
- Effectiveness in Symptom Relief: EECP has been shown to be effective in relieving symptoms of angina and improving the quality of life in patients with CAD. It can also be beneficial in some cases of heart failure, improving exercise tolerance and reducing symptoms.
- Stimulating Collateral Circulation: EECP can promote the development of collateral blood vessels, which can naturally bypass clogged arteries, improving blood flow to heart muscle.
- Avoiding Potential Complications of Invasive Procedures: Procedures like angioplasty and stenting carry risks such as restenosis (re-narrowing of the artery) and potential complications related to the stents themselves. EECP avoids these risks.
- Recovery Time and Hospitalization: EECP doesn’t require a hospital stay or a long recovery period, unlike surgical interventions. This can be particularly beneficial for patients who need to maintain their regular activities.
- Cost-Effectiveness: EECP can be more cost-effective than surgical interventions, which often require expensive hospital stays and post-operative care.
- Combination with Other Treatments: EECP can be used in combination with medication and lifestyle changes, often enhancing the overall treatment plan for CAD or heart failure.
- Patient Preference: Some patients may prefer to try a non-invasive approach before considering more invasive options.
However, it’s important to note that EECP is not suitable for all patients with CAD or heart failure. The decision to use EECP as a first-line treatment depends on the severity and nature of the disease, the presence of other health conditions, and the overall treatment goals. In many cases, particularly with severe blockages or advanced heart failure, interventional procedures or surgery might be the most appropriate and effective options. The treatment strategy should always be personalized and based on a thorough evaluation by a healthcare professional.
Why does it take a long time to derive benefit out of EECP, in contrast with Bypass surgery (CABG), the latter taking only a few days?
The difference in the time taken to derive benefits from Enhanced External Counterpulsation (EECP) compared to coronary artery bypass grafting (CABG, or bypass surgery) lies in the nature of these treatments and how they address coronary artery disease (CAD) or heart failure.
- Mechanism of Action:
- EECP: This treatment relies on the body’s natural healing mechanisms. It works by enhancing blood flow and encouraging the development of new blood vessels (collateral circulation) around blocked arteries. This process of angiogenesis (formation of new blood vessels) and adaptation of the cardiovascular system takes time, often several weeks.
- Bypass Surgery: CABG provides an immediate physical bypass around the blocked coronary arteries using grafts. This re-establishes blood flow to the heart muscle right after the surgery, leading to a quicker resolution of symptoms like chest pain (angina).
- Treatment Duration:
- EECP: Typically involves 35-40 sessions, each lasting about an hour, spread over 7-8 weeks. The gradual improvement in symptoms and cardiac function is noticed as the treatment progresses and often continues to improve even after the treatment course is completed.
- Bypass Surgery: It’s a single, albeit major, surgical procedure. Recovery from surgery and improvement in symptoms can begin soon after the operation, with many patients experiencing significant symptom relief within days or weeks.
- Biological Adaptation vs. Mechanical Solution:
- EECP: The benefits of EECP come from a biological adaptation process where the body enhances its own circulatory pathways. This is a more gradual process compared to a mechanical intervention.
- Bypass Surgery: Offers a direct and immediate mechanical solution to the problem of blocked arteries. The grafted arteries provide a new route for blood flow, bypassing the blockages almost immediately.
- Recovery and Rehabilitation:
- EECP: Since it’s non-invasive, there’s no surgical recovery period. The cumulative effect of the treatment builds up over time.
- Bypass Surgery: Although the surgical recovery can be significant, the direct rerouting of blood flow offers quicker symptom relief.
- Long-term Effects:
- EECP: The benefits of EECP, like improved angiogenesis and enhanced endothelial function, continue to develop and can have lasting effects even after the treatment course.
- Bypass Surgery: While the immediate effects are noticeable, long-term outcomes depend on various factors including the condition of the grafts, patient’s lifestyle, and adherence to medical advice.
In summary, EECP is a gradual, biological approach to improving heart health, relying on the body’s natural healing and adaptive mechanisms, while bypass surgery provides an immediate mechanical solution to circulatory blockages. The choice between these treatments depends on various factors including the severity of the disease, patient’s overall health, and specific medical circumstances.
Why is that EECP called Natural Bypass?
Enhanced External Counterpulsation (EECP) is often referred to as a “Natural Bypass” because of its ability to promote the development of new pathways for blood flow around blocked arteries in the heart, mimicking the effects of a surgical bypass but in a non-invasive manner. Here’s why EECP is associated with this term:
- Formation of Collateral Circulation: EECP can stimulate the opening and formation of small blood vessels in the heart, known as collateral vessels. These vessels can create natural bypasses around narrowed or blocked arteries, improving blood flow to heart muscle that is otherwise compromised.
- Non-Invasive Procedure: Unlike surgical bypass, which involves major surgery to graft arteries or veins from other parts of the body to bypass blocked coronary arteries, EECP is non-surgical. It uses external cuffs on the legs to enhance blood flow.
- Enhancing Blood Flow: During EECP, cuffs on the legs inflate and deflate in sync with the heart’s rhythm. This process increases blood flow back to the heart, particularly when the heart is relaxed, and decreases the heart’s workload.
- Mimicking the Effects of Bypass Surgery: By improving blood flow to the heart muscle, EECP mimics some of the benefits of coronary artery bypass graft (CABG) surgery. However, it’s important to note that EECP is not a replacement for bypass surgery in severe cases.
- Therapeutic Angiogenesis: The improved blood flow and decreased workload on the heart can promote angiogenesis, the formation of new blood vessels. This process is akin to creating natural bypass routes in the heart.
- Symptom Relief: EECP is primarily used for the treatment of angina (chest pain due to reduced blood flow to the heart muscles). It can relieve symptoms of heart disease, similar to how bypass surgery alleviates angina.
- Used for Patients Who Cannot Undergo Surgery: EECP is often a treatment option for patients who are not candidates for bypass surgery or angioplasty due to various medical reasons.
It’s important to note that while EECP is an effective treatment for certain heart conditions, particularly for symptom relief in chronic stable angina, it is not a substitute for coronary artery bypass grafting in cases where surgical intervention is necessary. EECP is often used when traditional treatments like surgery or medication are not viable or have not been fully effective. As with any medical treatment, the suitability of EECP for a patient should be evaluated by a healthcare professional.
Should I get hospitalized for EECP?
Enhanced External Counterpulsation (EECP) treatment typically does not require hospitalization. EECP is an outpatient procedure, meaning it’s performed in a setting where you can go home after each session. Here’s how the process usually works:
- Daily Sessions: EECP treatment involves regular sessions, often scheduled daily. Each session typically lasts about one hour and is usually conducted in a specialized clinic or outpatient department of a hospital.
- Series of Treatments: The full course of EECP treatment typically includes a series of sessions, commonly ranging from 35 to 40 sessions, spread over about 7 to 8 weeks.
- During the Session: During each session, you’ll lie on a bed, and large blood pressure-like cuffs will be wrapped around your legs and buttocks. These cuffs inflate and deflate in sync with your heartbeats, which enhances blood flow to your heart.
- Return Home Afterward: After each session, you can return to your home. There’s no need for an overnight stay in the hospital.
- Continuation of Normal Activities: Outside of your treatment sessions, you can typically continue with your regular daily activities, though your doctor might provide specific advice based on your individual health condition.
- Monitoring and Evaluation: Throughout the treatment course, your healthcare provider will monitor your progress and response to the treatment. This ensures that the therapy is effectively addressing your symptoms and any underlying conditions.
- Follow-Up Care: After completing the EECP treatment course, there will be follow-up evaluations to assess the long-term benefits and any need for additional treatment or lifestyle adjustments.
Since EECP is a non-invasive procedure and does not require recovery time like surgical treatments, it’s a convenient option for many patients who qualify for it. However, always consult with your healthcare provider for personalized advice and to understand how EECP fits into your overall treatment plan.
Why is that EECP is considered the first option if I have Coronary Artery Disease or Heart Failure, rather than Interventional procedures like Balloon Angioplasy, Stenting, Bypass surgery?
Enhanced External Counterpulsation (EECP) might be considered as a first-line treatment option for Coronary Artery Disease (CAD) or Heart Failure in certain circumstances, but this decision is highly individualized and depends on the specific details of each patient’s condition. Here’s why EECP might be preferred over more invasive interventional procedures like balloon angioplasty, stenting, or bypass surgery in some cases:
- Non-Invasiveness: EECP is a non-invasive procedure, which makes it a safer option, especially for patients who have high risks associated with surgical procedures. It doesn’t require anesthesia or incisions, reducing the risk of complications like bleeding or infection.
- Patient’s Overall Health and Suitability for Surgery: Patients with multiple comorbidities, advanced age, or other factors that make them high-risk candidates for surgery might benefit from EECP as a safer alternative.
- Effectiveness in Symptom Relief: EECP has been shown to be effective in relieving symptoms of angina and improving the quality of life in patients with CAD. It can also be beneficial in some cases of heart failure, improving exercise tolerance and reducing symptoms.
- Stimulating Collateral Circulation: EECP can promote the development of collateral blood vessels, which can naturally bypass clogged arteries, improving blood flow to heart muscle.
- Avoiding Potential Complications of Invasive Procedures: Procedures like angioplasty and stenting carry risks such as restenosis (re-narrowing of the artery) and potential complications related to the stents themselves. EECP avoids these risks.
- Recovery Time and Hospitalization: EECP doesn’t require a hospital stay or a long recovery period, unlike surgical interventions. This can be particularly beneficial for patients who need to maintain their regular activities.
- Cost-Effectiveness: EECP can be more cost-effective than surgical interventions, which often require expensive hospital stays and post-operative care.
- Combination with Other Treatments: EECP can be used in combination with medication and lifestyle changes, often enhancing the overall treatment plan for CAD or heart failure.
- Patient Preference: Some patients may prefer to try a non-invasive approach before considering more invasive options.
However, it’s important to note that EECP is not suitable for all patients with CAD or heart failure. The decision to use EECP as a first-line treatment depends on the severity and nature of the disease, the presence of other health conditions, and the overall treatment goals. In many cases, particularly with severe blockages or advanced heart failure, interventional procedures or surgery might be the most appropriate and effective options. The treatment strategy should always be personalized and based on a thorough evaluation by a healthcare professional.
Why does it take a long time to derive benefit out of EECP, in contrast with Bypass surgery (CABG), the latter taking only a few days?
The difference in the time taken to derive benefits from Enhanced External Counterpulsation (EECP) compared to coronary artery bypass grafting (CABG, or bypass surgery) lies in the nature of these treatments and how they address coronary artery disease (CAD) or heart failure.
- Mechanism of Action:
- EECP: This treatment relies on the body’s natural healing mechanisms. It works by enhancing blood flow and encouraging the development of new blood vessels (collateral circulation) around blocked arteries. This process of angiogenesis (formation of new blood vessels) and adaptation of the cardiovascular system takes time, often several weeks.
- Bypass Surgery: CABG provides an immediate physical bypass around the blocked coronary arteries using grafts. This re-establishes blood flow to the heart muscle right after the surgery, leading to a quicker resolution of symptoms like chest pain (angina).
- Treatment Duration:
- EECP: Typically involves 35-40 sessions, each lasting about an hour, spread over 7-8 weeks. The gradual improvement in symptoms and cardiac function is noticed as the treatment progresses and often continues to improve even after the treatment course is completed.
- Bypass Surgery: It’s a single, albeit major, surgical procedure. Recovery from surgery and improvement in symptoms can begin soon after the operation, with many patients experiencing significant symptom relief within days or weeks.
- Biological Adaptation vs. Mechanical Solution:
- EECP: The benefits of EECP come from a biological adaptation process where the body enhances its own circulatory pathways. This is a more gradual process compared to a mechanical intervention.
- Bypass Surgery: Offers a direct and immediate mechanical solution to the problem of blocked arteries. The grafted arteries provide a new route for blood flow, bypassing the blockages almost immediately.
- Recovery and Rehabilitation:
- EECP: Since it’s non-invasive, there’s no surgical recovery period. The cumulative effect of the treatment builds up over time.
- Bypass Surgery: Although the surgical recovery can be significant, the direct rerouting of blood flow offers quicker symptom relief.
- Long-term Effects:
- EECP: The benefits of EECP, like improved angiogenesis and enhanced endothelial function, continue to develop and can have lasting effects even after the treatment course.
- Bypass Surgery: While the immediate effects are noticeable, long-term outcomes depend on various factors including the condition of the grafts, patient’s lifestyle, and adherence to medical advice.
In summary, EECP is a gradual, biological approach to improving heart health, relying on the body’s natural healing and adaptive mechanisms, while bypass surgery provides an immediate mechanical solution to circulatory blockages. The choice between these treatments depends on various factors including the severity of the disease, patient’s overall health, and specific medical circumstances.