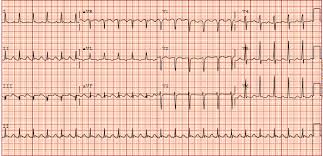
Picture a detective, keenly studying a series of clues to solve a mystery. In the realm of heart health, an ECG (Electrocardiogram) plays a similar role. It’s a simple test that traces the heart’s electrical activity, capturing its story through unique waves and lines on a graph.
But what heart secrets can the ECG unveil? Quite a few, actually! Here are some of the mysteries it helps decipher.

Alright, gather ’round, folks! Let me tell you about this detective gadget that’s straight out of a spy movie—it’s the Electrocardiogram, the ubiquitous ECG or EKG, and it’s cooler than a cucumber!
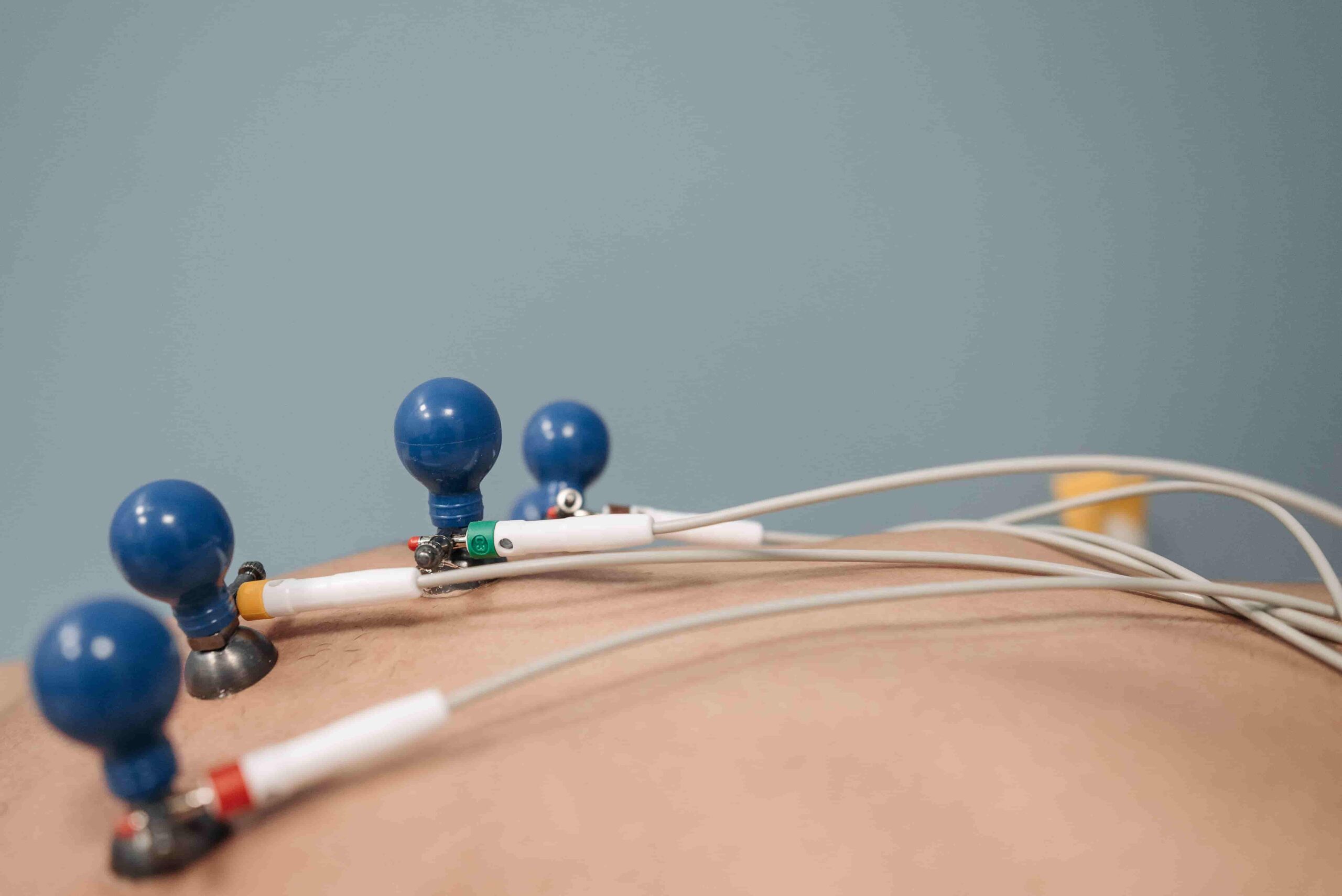
First off, it’s like lightning-fast and as non-invasive as a gentle breeze. Just slap on some teeny electrodes, and bam! Doctors are suddenly Sherlock Holmes, unraveling the heart’s mysteries faster than you can say “heart palpitations.”
Now, let’s talk about what this bad boy can uncover:
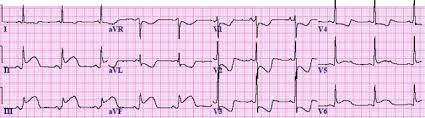
- Arrhythmias: Think of these as the heart’s funky dance moves. Whether it’s doing the salsa too fast or the cha-cha too slow, the ECG spots every misstep.
- Heart Attacks: Oh, the drama! If there’s been a heartbreak—err, I mean, heart attack—the ECG waves spill the beans faster than gossip at a high school reunion.
- Blocked Arteries: It’s like a traffic jam in your heart’s highway. If there’s a detour or a roadblock, the ECG sniffs it out quicker than a bloodhound on a scent.
- Structural Shenanigans: Sometimes, the heart’s playing Tetris with its walls. But fear not! The ECG picks up on any architectural oddities, giving doctors the heads-up on potential issues.
So, there you have it, folks! The ECG—your heart’s trusty sidekick in the battle against sneaky health hiccups.
It’s like having a superhero in scrubs on your side!
FAQs on Arrhythmias
What is the meaning of arrhythmia?
Heart arrhythmia refers to an irregular heartbeat, where the heart’s rhythm deviates from its normal pattern. It can manifest as a heartbeat that’s too fast, too slow, or erratic, disrupting the efficient flow of blood throughout the body. Arrhythmias can range from harmless to life-threatening, often requiring medical attention for diagnosis and management. They are caused by various factors, including heart disease, stress, genetics, and certain medications, making awareness and timely intervention crucial for heart health..
Why are arrhythmias caused?
Heart arrhythmias can be caused by a variety of factors, often involving changes to the heart’s electrical system. Some common causes include:
- Heart Conditions: Existing heart conditions such as coronary artery disease, heart valve disease, heart failure, previous heart surgery, and cardiomyopathy can lead to arrhythmias.
- Electrolyte Imbalances: Imbalances in electrolytes, such as potassium, sodium, calcium, and magnesium, which help conduct electrical impulses in the heart, can cause arrhythmias.
- High Blood Pressure: Chronic high blood pressure can increase the risk of developing an arrhythmia.
- Congenital Heart Defects: People born with heart defects may be more likely to have arrhythmias.
- Thyroid Problems: Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) can lead to heart rhythm problems.
- Substance Use: Excessive alcohol consumption, smoking, caffeine, certain medications (like over-the-counter cold and allergy drugs), and recreational drugs can trigger arrhythmias.
- Diabetes: Diabetes, especially when not well-controlled, increases the risk of arrhythmias.
- Stress and Anxiety: High levels of stress or anxiety can lead to temporary arrhythmias.
- Age: The likelihood of developing an arrhythmia increases with age, as the heart undergoes changes.
- Genetics: Some types of arrhythmias can be inherited, meaning a family history may increase the risk.
- Sleep Apnea: Untreated sleep apnea can increase the risk of arrhythmias.
It’s important to note that sometimes the exact cause of an arrhythmia can’t be identified, which is referred to as idiopathic arrhythmia. Regular check-ups and a healthy lifestyle can help manage risks associated with heart arrhythmias.
Should I worry about these Arrhythmias?
Whether or not to worry about an arrhythmia depends on its type, severity, underlying cause, and the presence of other heart conditions. Arrhythmias can range from benign to life-threatening, so understanding the specifics is crucial:
- Benign Arrhythmias: Some arrhythmias, like occasional premature atrial contractions (PACs) or premature ventricular contractions (PVCs), are generally harmless and common in healthy people. They might not require treatment unless they are frequent or cause significant symptoms.
- Potentially Serious Arrhythmias: Conditions like atrial fibrillation (AFib), ventricular tachycardia, and ventricular fibrillation are more serious. AFib, for example, increases the risk of stroke and may require medication to control the heart rate, prevent clots, or both.
- Symptoms and Risks: If you experience symptoms like palpitations, dizziness, shortness of breath, chest pain, or fainting, it’s important to seek medical advice. The risk posed by an arrhythmia often depends on other factors like the presence of heart disease, the effectiveness of the heart’s pumping action, and your overall health.
- Lifestyle Factors: For some arrhythmias, lifestyle changes like reducing caffeine and alcohol intake, quitting smoking, managing stress, and maintaining a healthy weight can significantly reduce their occurrence and severity.
- Regular Monitoring and Treatment: For more serious conditions, regular monitoring and treatment, which can include medications, lifestyle changes, or procedures like catheter ablation or the implantation of a pacemaker or defibrillator, might be necessary.
In summary, while some arrhythmias are harmless and require no treatment, others can be serious and increase the risk of more severe health problems. It’s always best to consult with a healthcare professional for a proper diagnosis and treatment plan. Regular check-ups and paying attention to your body’s signals are key to addressing heart health concerns effectively.
Consult your doctor about these arrhythmia and take remedial measures, if required.
How to control these arrhythmias?
Controlling arrhythmias often involves a combination of medication, lifestyle changes, and in some cases, medical devices or procedures. The specific approach depends on the type of arrhythmia, its severity, underlying causes, and the patient’s overall health. Here are some common medical measures:
- Medications:
- Antiarrhythmic Drugs: Used to control the heart rate and rhythm. Examples include amiodarone, flecainide, and sotalol.
- Beta-Blockers: Such as metoprolol and atenolol, reduce the heart rate and are often used for atrial fibrillation and other supraventricular tachycardias.
- Calcium Channel Blockers: Like diltiazem and verapamil, these also help control heart rate.
- Blood Thinners (Anticoagulants): For arrhythmias like atrial fibrillation, which increase the risk of blood clots, drugs like warfarin or newer agents (e.g., dabigatran, rivaroxaban) might be prescribed.
- Medical Devices:
- Pacemakers: For arrhythmias causing the heart to beat too slowly, a pacemaker can be implanted to maintain a normal heart rate.
- Implantable Cardioverter Defibrillators (ICDs): For life-threatening ventricular arrhythmias, an ICD can provide a life-saving shock or pacing to restore normal rhythm.
- Procedures/Surgeries:
- Catheter Ablation: A minimally invasive procedure used to destroy small areas of heart tissue that are causing arrhythmias.
- Cardioversion: A procedure where an electrical shock is given to the heart to reset its rhythm back to normal. Often used in emergency situations or as a planned procedure.
- Maze Surgery: A more invasive surgical procedure for atrial fibrillation, where a series of precise incisions in the heart’s atria are made to prevent abnormal electrical signals.
- Lifestyle Changes:
- Diet and Exercise: A healthy diet and regular exercise can improve heart health and reduce arrhythmia risk.
- Managing Risk Factors: Controlling high blood pressure, diabetes, and cholesterol, and quitting smoking.
- Stress Reduction: Techniques like yoga, meditation, and counseling can help manage stress, which is a potential trigger for some arrhythmias.
- Regular Monitoring:
- Routine check-ups and possibly wearing a Holter monitor or using a portable ECG device to record and track heart rhythms.
It’s important to work closely with a healthcare provider to determine the best treatment plan based on individual needs and the specifics of the arrhythmia
Do I need an Artificial Pace-maker if I have been detected with an arrhythmia?
Not necessarily always!
Controlling arrhythmias often involves a combination of medication, lifestyle changes, and in some cases, medical devices or procedures.
The specific approach depends on the type of arrhythmia, its severity, underlying causes, and the patient’s overall health. Here are some common medical measures:
It’s important to work closely with a healthcare provider to determine the best treatment plan based on individual needs and the specifics of the arrhythmia
FAQs on Heart Attack
What is a Heart Attack?
A heart attack, also known as a myocardial infarction, occurs when the flow of blood to a part of the heart is blocked, usually by a blood clot. This blockage, often caused by a buildup of fat, cholesterol, and other substances, forms plaque in the coronary arteries that feed the heart (coronary artery disease). When a plaque in a heart artery breaks, a blood clot forms around the plaque. If the clot blocks the blood flow completely, the heart muscle becomes starved for oxygen. Within a short time, death of heart muscle cells occurs, causing permanent damage.
Why does a Heart Attack occur?
A heart attack, medically known as a myocardial infarction, occurs when there is a sudden blockage of blood flow to a part of the heart muscle. This blockage typically happens due to the following reasons:
- Coronary Artery Disease (CAD): The most common cause of heart attacks is coronary artery disease. CAD is a condition in which the coronary arteries, which supply oxygen-rich blood to the heart muscle, become narrowed or blocked by a buildup of fatty deposits called plaque. Over time, these plaques can rupture, causing a blood clot to form at the site of the rupture.
- Blood Clot Formation: When a plaque ruptures, it exposes the inner layer of the artery to the bloodstream. Platelets in the blood can then stick to this exposed area and form a blood clot. If the blood clot becomes large enough, it can completely block the artery, cutting off the blood supply to a part of the heart muscle.
- Spasm of the Coronary Artery: In some cases, a heart attack can occur due to a sudden spasm or contraction of a coronary artery. This can temporarily reduce or completely block blood flow to the heart muscle, leading to a heart attack. Coronary artery spasms can be triggered by various factors, including smoking, drug use, and stress.
- Artery Dissection: Rarely, a heart attack can be caused by a tear in the coronary artery wall, known as coronary artery dissection. This tear can obstruct blood flow and result in a heart attack.
The lack of oxygen-rich blood reaching a part of the heart muscle can lead to tissue damage and cell death. The severity of a heart attack depends on factors such as the size of the affected area and how quickly medical intervention is provided. Prompt treatment, often involving procedures like angioplasty and stent placement to restore blood flow, can help minimize heart muscle damage and improve the chances of recovery.
It’s important to note that certain risk factors, such as high blood pressure, high cholesterol, smoking, diabetes, and a family history of heart disease, can increase the likelihood of developing coronary artery disease and experiencing a heart attack. Lifestyle changes and medical interventions can help manage these risk factors and reduce the risk of heart attacks.
Are Heart Attacks fatal always?
Heart attacks can vary in severity, and not all heart attacks are fatal. The outcome of a heart attack depends on several factors, including the size and location of the blocked coronary artery, the extent of damage to the heart muscle, how quickly medical treatment is received, and the overall health of the individual.
While heart attacks can be life-threatening, many people survive them with prompt medical intervention and appropriate treatment. In fact, advances in medical care and technology have improved the prognosis for individuals who experience heart attacks.
Some possible outcomes of a heart attack include:
- Survival with Minor Damage: If medical treatment is received quickly and the blockage in the coronary artery is cleared, it is possible for an individual to survive a heart attack with minimal damage to the heart muscle. In such cases, the heart can often recover and function relatively normally.
- Survival with Moderate Damage: Some heart attacks may result in moderate damage to the heart muscle. While this can affect heart function, it may still be manageable with medical therapy and lifestyle changes.
- Severe Damage or Heart Failure: In cases where there is extensive damage to the heart muscle, heart failure can occur. This can lead to long-term complications and a decreased quality of life. However, even in cases of severe damage, medical treatment and interventions like heart bypass surgery or heart transplant may be options to improve outcomes.
- Fatal Outcome: Unfortunately, some heart attacks can be fatal. If the blockage in a coronary artery is not promptly treated, or if the heart attack leads to severe complications like cardiac arrest or arrhythmias that cannot be reversed, it can result in death.
It’s important to recognize the signs and symptoms of a heart attack, such as chest pain or discomfort, shortness of breath, lightheadedness, nausea, and pain radiating to the arms, neck, jaw, or back. If you or someone you are with experiences these symptoms, it is crucial to seek immediate medical attention by calling 911 or the emergency services in your area. Early intervention can significantly increase the chances of surviving a heart attack and minimizing heart muscle damage. Additionally, lifestyle changes and ongoing medical care can help reduce the risk of future heart events.
What are the outcomes of a non-fatal Heart Attack?
The outcomes of a non-fatal heart attack, also known as a myocardial infarction (MI), can vary depending on several factors, including the extent of damage to the heart muscle, the individual’s overall health, the promptness of medical treatment, and subsequent lifestyle changes and medical management. Here are some potential outcomes following a non-fatal heart attack:
- Recovery with Minor Damage: In some cases, a non-fatal heart attack may cause minor damage to the heart muscle. With prompt medical intervention and appropriate treatment, the heart muscle can often recover, and the individual may experience a good quality of life with minimal long-term effects.
- Recovery with Moderate Damage: If the heart attack results in moderate damage to the heart muscle, the individual may experience some reduction in heart function. However, with proper medical management, lifestyle changes (such as quitting smoking, adopting a heart-healthy diet, and regular exercise), and adherence to prescribed medications, it is often possible to lead a relatively normal life. Cardiac rehabilitation programs can be beneficial in optimizing recovery and improving heart health.
- Heart Failure: In cases where the heart attack causes significant damage to the heart muscle, heart failure can occur. Heart failure is a condition in which the heart’s ability to pump blood effectively is compromised. Treatment for heart failure may include medications, lifestyle changes, and, in severe cases, advanced interventions such as heart transplant or mechanical assist devices (like ventricular assist devices or VADs).
- Complications: Some individuals may experience complications following a heart attack, such as arrhythmias (irregular heart rhythms), heart valve problems, or blood clots. These complications may require additional treatment, including medications, procedures, or surgeries.
- Lifestyle Changes: After a non-fatal heart attack, healthcare providers typically recommend significant lifestyle changes to reduce the risk of future heart events. This often includes adopting a heart-healthy diet, quitting smoking, managing blood pressure and cholesterol levels, maintaining a healthy weight, engaging in regular physical activity, and managing stress.
- Medications: Many people who have experienced a heart attack are prescribed medications to manage risk factors and improve heart health. Common medications include aspirin, beta-blockers, ACE inhibitors, statins, and antiplatelet drugs, among others.
It’s important for individuals who have had a heart attack to follow their healthcare provider’s recommendations, attend regular follow-up appointments, and take prescribed medications as directed. With appropriate medical care and lifestyle modifications, many people can lead fulfilling lives after a non-fatal heart attack and reduce their risk of future cardiac events. The key is early intervention, adherence to treatment plans, and ongoing cardiovascular care.
What is Chronic Coronary Syndrome (CCS)?
Chronic Coronary Syndrome (CCS), formerly known as chronic stable angina or stable ischemic heart disease, is a cardiovascular condition characterized by persistent reduced blood flow to the heart muscle due to atherosclerosis and coronary artery disease (CAD). Unlike acute coronary syndrome (ACS), which includes conditions like unstable angina and myocardial infarction (heart attack), CCS refers to the more chronic and stable nature of angina symptoms.
Key features and characteristics of Chronic Coronary Syndrome (CCS) include:
- Angina Pectoris: The primary symptom of CCS is angina, which is chest discomfort or pain that occurs when the heart muscle does not receive enough oxygen due to reduced blood flow in the coronary arteries. Angina may also manifest as discomfort in the arms, neck, jaw, shoulder, back, or stomach. This discomfort typically occurs during physical activity or emotional stress and is relieved by rest or medication.
- Stable Symptoms: Unlike unstable angina, which is characterized by unpredictable and often worsening symptoms, CCS symptoms are stable and predictable. They typically occur with consistent triggers, such as exertion or emotional stress, and tend to follow a similar pattern over time.
- Atherosclerosis: CCS is primarily caused by the buildup of atherosclerotic plaques within the coronary arteries. These plaques narrow the arteries and reduce blood flow to the heart muscle. While the disease process is chronic, it can gradually worsen over time.
- Diagnosis: CCS is diagnosed based on the patient’s medical history, symptoms, and various diagnostic tests, including electrocardiography (ECG or EKG), stress tests, coronary angiography, and imaging studies like coronary CT angiography or cardiac MRI.
- Treatment: The management of CCS aims to relieve symptoms, improve quality of life, and reduce the risk of future cardiovascular events. Treatment may involve lifestyle changes (such as quitting smoking, adopting a heart-healthy diet, and regular exercise), medications (such as nitroglycerin, beta-blockers, calcium channel blockers, and antiplatelet drugs), and, in some cases, revascularization procedures like angioplasty and stent placement or coronary artery bypass grafting (CABG).
- Risk Factor Management: Managing risk factors for atherosclerosis and CAD is essential in the management of CCS. This includes controlling high blood pressure, managing cholesterol levels, controlling diabetes, and addressing other modifiable risk factors.
It’s important for individuals with CCS to work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific needs and risk factors. Regular follow-up appointments and adherence to the prescribed treatment and lifestyle recommendations are crucial for managing CCS effectively and reducing the risk of complications.
What is Acute Coronary Syndrome (ACS)?
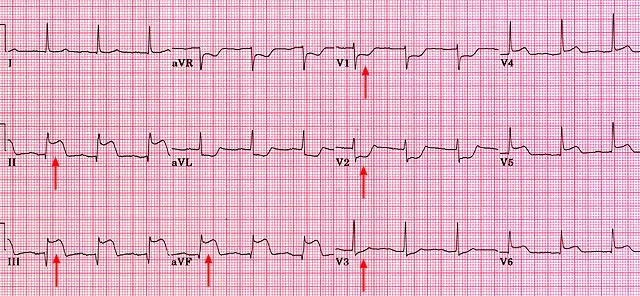
Acute Coronary Syndrome (ACS) is a term used to describe a group of serious and potentially life-threatening cardiovascular conditions that are caused by a sudden reduction or blockage of blood flow to the heart muscle. ACS encompasses a range of clinical presentations, including unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI), with STEMI being the most severe form.
Here are the key components of Acute Coronary Syndrome:
- Unstable Angina: Unstable angina is characterized by chest pain or discomfort that occurs at rest, with minimal exertion, or in an unpredictable pattern. It is considered unstable because the symptoms are more severe, prolonged, and occur with less predictable triggers than stable angina. Unstable angina is a warning sign that a heart attack may be imminent.
- NSTEMI (Non-ST-Segment Elevation Myocardial Infarction): NSTEMI is a type of heart attack that occurs when there is a partial blockage or temporary clot in one or more coronary arteries, resulting in a reduced blood supply to a portion of the heart muscle. This condition is diagnosed based on specific changes in blood markers (troponin) that indicate heart muscle damage.
- STEMI (ST-Segment Elevation Myocardial Infarction): STEMI is the most severe form of ACS and represents a complete blockage of a coronary artery, typically due to a blood clot. It is considered a true heart attack, and immediate medical attention is required. ECG (electrocardiogram) changes, particularly ST-segment elevation, are characteristic of STEMI. Prompt treatment is crucial to restore blood flow to the affected area of the heart muscle and minimize damage.
The underlying cause of ACS is often atherosclerosis, a condition characterized by the buildup of fatty deposits (atherosclerotic plaques) in the coronary arteries. These plaques can rupture or become unstable, leading to the formation of blood clots that can partially or completely block blood flow to the heart muscle.
Treatment for ACS involves rapid evaluation and intervention, including medications to relieve chest pain, stabilize blood flow, and prevent further clot formation, as well as revascularization procedures such as angioplasty and stent placement or coronary artery bypass surgery (CABG). The choice of treatment depends on the specific diagnosis and the severity of the condition.
ACS is a medical emergency, and anyone experiencing symptoms such as chest pain or discomfort, shortness of breath, nausea, or lightheadedness should seek immediate medical attention by calling 911 or the emergency services in their area. Early intervention can significantly improve outcomes and reduce the risk of complications associated with ACS, including heart muscle damage, heart failure, and life-threatening arrhythmias.
What are the methods of treatment in acute coronary syndrome?
The treatment of Acute Coronary Syndrome (ACS) involves a combination of medical therapies and, in some cases, interventional or surgical procedures. The specific treatment approach depends on the type of ACS (unstable angina, NSTEMI, or STEMI), the severity of the condition, the patient’s overall health, and other individual factors. Here are the main methods of treatment for ACS:
- Medications:a. Antiplatelet Agents: These drugs prevent blood clot formation. Common antiplatelet medications include aspirin and P2Y12 inhibitors (such as clopidogrel, prasugrel, or ticagrelor).b. Anticoagulants: These medications, such as heparin or low-molecular-weight heparin, help prevent further blood clot formation and growth.c. Nitroglycerin: Nitroglycerin can be used to relieve chest pain by dilating blood vessels and improving blood flow to the heart.d. Pain Relievers: Non-opioid analgesics like acetaminophen can help manage chest discomfort.e. Beta-Blockers: These medications, like metoprolol or carvedilol, can reduce heart rate and blood pressure, decreasing the workload on the heart.f. ACE Inhibitors or ARBs: These drugs are used to manage blood pressure and reduce the strain on the heart.g. Statin Medications: Statins like atorvastatin or rosuvastatin are used to lower cholesterol levels and reduce the risk of further plaque buildup.h. Other Medications: Additional medications may be prescribed based on the patient’s specific needs and conditions, such as diabetes management, arrhythmia control, and heart failure treatment.
- Revascularization Procedures:a. Percutaneous Coronary Intervention (PCI): PCI, commonly known as angioplasty, involves the use of a catheter to open blocked coronary arteries. A stent may be inserted to help keep the artery open.b. Coronary Artery Bypass Grafting (CABG): CABG surgery may be recommended for individuals with complex or multiple blockages. During CABG, a surgeon grafts a healthy blood vessel (usually from the patient’s leg or chest) to bypass the blocked artery, restoring blood flow to the heart.
- Cardiac Rehabilitation: After ACS treatment, a cardiac rehabilitation program may be recommended. This program includes supervised exercise, education on heart-healthy lifestyle changes, and emotional support to improve recovery and reduce the risk of future cardiovascular events.
- Lifestyle Modifications: Adopting a heart-healthy lifestyle is essential for long-term management. This includes quitting smoking, following a heart-healthy diet, managing weight, controlling blood pressure, and engaging in regular physical activity.
- Ongoing Medication Management: Many individuals with ACS will need to take medications long-term to manage risk factors and prevent future cardiovascular events. It’s crucial to adhere to prescribed medications and follow up with healthcare providers as recommended.
- Psychosocial Support: Managing the emotional and psychological impact of ACS is essential. Support from healthcare professionals, family, and support groups can be valuable in coping with the emotional aspects of the condition.
Treatment for ACS should be individualized, and decisions should be made in consultation with a healthcare provider. Prompt and appropriate treatment is critical to improve outcomes and reduce the risk of complications. If you or someone you know experiences symptoms of ACS, such as chest pain or discomfort, seek immediate medical attention by calling 911 or the emergency services in your area.
FAQs on Blocked Arteries
Why and What arteries are often blocked in the human body?
Atherosclerosis is the technical word. It simply means “a porridge-like thickening” in Greek. This is a degenerative pathological process. It starts very early in life and is progressive. The slope of the disease progression varies in different individuals and sex. The manifestations of Atherosclerosis is throughout the body. Depending on where it occurs, different organ systems are involved as end-organ damage takes place.
Why are the common arteries that are blocked?
- Heart’s Coronary Arteries, resulting in Coronary Artery Disease (CAD) and Heart Attacks,
- Brain’s Cerebral Arteries, resulting in Brain Attacks or Stroke,
- Kidney’s Renal Arteries, resulting in Acute Kidney Failure,
- Intestinal arteries, resulting in Gangrene of the Gut,
- Peripheral arteries of the Legs, resulting in Peripheral Arterial Disease (PAD).
Should I worry about these blocked arteries?
Of course YES, you should be concerned about blocked arteries in the heart, brain, kidneys, and intestines, as they can lead to serious health problems. Here’s a brief overview of the issues associated with blockages in these areas:
- Heart (Coronary Arteries): Blockages in the coronary arteries can lead to a heart attack (myocardial infarction). This occurs when the blood supply to a part of the heart is interrupted, causing damage or death to the heart muscle. Symptoms include chest pain, shortness of breath, and discomfort in the arms, back, neck, jaw, or stomach. Sometimes, diaseases loke Diabetes can totally mask these symptoms.
- Brain (Cerebral Arteries): Blocked arteries in the brain can cause a stroke. There are two main types of stroke: ischemic (caused by a blockage) and hemorrhagic (caused by a burst blood vessel). Symptoms of a stroke include sudden numbness or weakness in the face, arm, or leg (especially on one side of the body), confusion, trouble speaking or understanding speech, vision problems, difficulty walking, dizziness, and loss of balance or coordination.
- Kidneys (Renal Arteries): Blockages in the renal arteries can lead to renal artery stenosis, which can cause high blood pressure and kidney damage. In severe cases, this can lead to kidney failure, requiring dialysis or a kidney transplant.
- Intestines (Mesenteric Arteries): Blockage in the arteries supplying the intestines can lead to mesenteric ischemia. This condition can cause severe abdominal pain, nausea, vomiting, and eventually, tissue death. It’s a medical emergency that requires immediate attention.
- Peripheral Arterial Disease: Leg arteries could be involved in atherosclerotic process, resulting in Intermittent Claudication. Whe you walk up certain distance, you get a sharp ache in the muscles of your legs, relieved when you stop walking and take a rest. If progressive and attains a critical magnitude, this could cause death of tissues in the toes, legs (Gangrene) and may result in loss of these structures by amputation.
Prevention and early detection of arterial blockages are key. This involves managing risk factors like high blood pressure, high cholesterol, diabetes, obesity, and smoking. Regular exercise, a healthy diet, and regular medical check-ups are also important for cardiovascular health.
If you have any risk factors for arterial blockages or experience symptoms suggestive of a blockage, you should consult a healthcare professional for an evaluation and appropriate management.
What if I smoke? Is smoking harmful? Could arteries get blocked if I smoked?
Yes, smoking is extremely harmful to health. It is a very important “modifiable risk factor” for Coronary Artery Disease (CAD). It’s one of the leading causes of preventable death worldwide. The adverse effects of smoking affect almost every organ in the body and significantly increase the risk of numerous diseases. Here are some key points about the harm caused by smoking:
- Cardiovascular Diseases: Smoking is a major cause of cardiovascular diseases, including heart attacks, strokes, and peripheral vascular disease. Chemicals in tobacco can damage the heart and blood vessels, leading to narrowing of the arteries (atherosclerosis), which can ultimately lead to a heart attack or stroke.
- Cancer: Smoking is a leading cause of cancer and death from cancer. It is directly linked to lung cancer and is also associated with cancer of the mouth, throat, larynx, esophagus, stomach, pancreas, liver, kidney, bladder, cervix, and some leukemias.
- Respiratory Diseases: Smoking damages the lungs and airways, causing chronic obstructive pulmonary disease (COPD), which includes conditions like chronic bronchitis and emphysema. Smokers are also more likely to have respiratory infections like pneumonia.
- Other Health Risks: Smoking increases the risk of osteoporosis, cataracts, and macular degeneration. It affects reproductive health, leading to reduced fertility and increased risk of birth defects. In men, it can cause erectile dysfunction.
- Secondhand Smoke: Exposure to secondhand smoke is also harmful, especially to children and pregnant women. It increases the risk of developing heart disease, lung cancer, and respiratory conditions.
- Addiction: Nicotine in cigarettes is highly addictive, making it difficult for smokers to quit. However, quitting smoking has immediate and long-term health benefits, reducing the risks of diseases associated with smoking and improving overall health.
Given these risks, it’s strongly advised to quit smoking. There are many resources available to help with quitting, including medications, nicotine replacement therapy, and support groups. The benefits of quitting smoking begin almost immediately and continue to improve health over time. If you’re considering quitting, it’s a good idea to consult with a healthcare provider for guidance and support tailored to your individual needs.
What if I reduce the number of cigarettes smoked ? Still harmful?
As far as the risks of smoking on the Cardio-vascular system is concerned, it is an established fact that there is no difference of 2 or 20 cigarettes are smoked per day. The risk ratio remains the same.
What about Beedi Smoking?
Yes, beedi smoking can significantly increase the risk of a heart attack (myocardial infarction) and other cardiovascular problems. Beedis, also known as bidi or biri, are a type of traditional hand-rolled cigarettes that are popular in some parts of the world, particularly in India and parts of South Asia.
Beedis are made by rolling tobacco in a tendu or temburni leaf and are often flavored. While they may seem less harmful than regular cigarettes, beedis are not a safe alternative, and they carry several health risks, including cardiovascular risks:
- Nicotine: Beedis contain nicotine, a highly addictive substance. Nicotine raises heart rate and blood pressure, increasing the workload on the heart and potentially leading to hypertension (high blood pressure).
- Toxic Chemicals: Beedi smoke contains many of the same toxic chemicals found in regular cigarettes, including tar, carbon monoxide, and various carcinogens. These chemicals can damage blood vessels and promote the development of atherosclerosis (narrowing and hardening of the arteries), increasing the risk of coronary artery disease.
- Carbon Monoxide: Beedi smoke contains carbon monoxide, which can reduce the amount of oxygen that the blood carries to the heart and other organs. This can strain the heart and increase the risk of heart attacks.
- Secondhand Smoke: People exposed to secondhand smoke from beedis are also at risk of cardiovascular problems, including heart attacks. The smoke can have harmful effects on the cardiovascular system of nonsmokers.
- Duration of Smoking: Beedi smokers often smoke multiple beedis throughout the day, which can lead to prolonged exposure to harmful chemicals and increased cardiovascular risk over time.
It’s essential to recognize that beedis are not a safe or healthy smoking option. Quitting smoking altogether is the best way to reduce the risk of heart attacks and other smoking-related health issues. If you or someone you know smokes beedis and is concerned about their cardiovascular health, seeking support and resources to quit smoking is strongly recommended. Quitting smoking can lead to significant improvements in cardiovascular health and overall well-being.
FAQs on Structural Issues
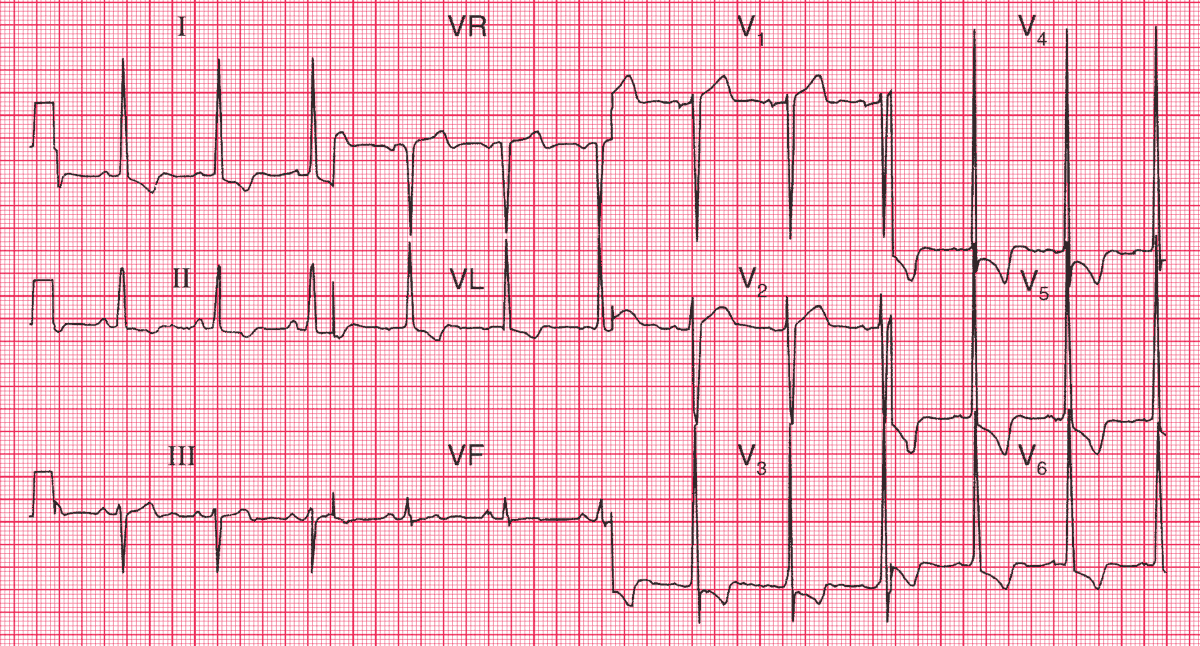
What are the structural changes that take place in the heart as cause / effect of disease processes?
Structural issues in the heart can occur as both a cause and an effect of various disease processes. These structural problems can have a significant impact on heart function and overall health. Here are some common structural issues that can occur in the heart:
- Coronary Artery Disease (CAD):
- Atherosclerosis: The buildup of fatty plaques in the coronary arteries can narrow or block them, reducing blood flow to the heart muscle. This can lead to ischemia (insufficient blood supply) and structural changes in the heart.
- Coronary Artery Stenosis: Severe narrowing or blockage of coronary arteries can result in reduced blood flow to the heart and may lead to heart muscle damage or infarction (heart attack).
- Heart Attack (Myocardial Infarction):
- A heart attack can cause structural damage to the heart muscle, resulting in areas of scar tissue (myocardial fibrosis). Over time, this can weaken the heart and affect its ability to pump blood effectively, leading to heart failure.
- Heart Failure:
- Dilated Cardiomyopathy: In this condition, the heart chambers become enlarged (dilated), and the heart muscle weakens, leading to reduced pumping capacity.
- Hypertrophic Cardiomyopathy: This condition is characterized by abnormal thickening of the heart muscle, which can obstruct blood flow out of the heart and impair its function.
- Restrictive Cardiomyopathy: In restrictive cardiomyopathy, the heart muscle becomes stiff and less compliant, making it harder for the heart to fill with blood.
- Valvular Heart Disease:
- Valve Stenosis: Narrowing (stenosis) of heart valves, such as the aortic or mitral valve, can obstruct blood flow and result in structural changes to the heart.
- Valve Regurgitation: In valve regurgitation (insufficiency), the valves do not close properly, allowing blood to leak backward. Over time, this can lead to chamber enlargement and changes in the heart’s structure.
- Congenital Heart Defects:
- Structural abnormalities present at birth can affect the heart’s structure and function, leading to conditions such as atrial septal defects, ventricular septal defects, or complex congenital heart malformations.
- Hypertension (High Blood Pressure):
- Long-term, uncontrolled high blood pressure can lead to structural changes in the heart, such as left ventricular hypertrophy (enlargement and thickening of the heart’s left ventricle). This can impair the heart’s ability to pump efficiently.
- Pericardial Disease:
- Conditions like pericarditis (inflammation of the pericardium) or constrictive pericarditis (scarring and thickening of the pericardium) can affect the heart’s ability to expand and contract properly.
- Arrhythmogenic Right Ventricular Dysplasia (ARVD):
- ARVD is a rare genetic disorder that can lead to the replacement of heart muscle with fatty or fibrous tissue, affecting the heart’s structure and electrical function.
- Cardiac Tumors:
- Rarely, tumors can develop in the heart, affecting its structural integrity and potentially obstructing blood flow or causing other complications.
- Aortic Aneurysm and Dissection:
- Structural abnormalities of the aorta, such as aneurysms (weakened and bulging areas) or dissections (tears in the aortic wall), can impact the heart’s function and require surgical intervention.
These structural issues in the heart can vary in severity and may require medical treatment, lifestyle modifications, medications, or surgical procedures to manage or correct. Regular medical evaluations and appropriate management are essential to address these conditions and minimize their impact on heart function and overall health.
Why are these structural changes caused?
Structural changes in the heart can be caused by a variety of factors and underlying conditions. The specific causes of these structural changes can vary depending on the type of structural issue and the individual’s unique circumstances. Here are some common reasons why structural changes occur in the heart:
- Coronary Artery Disease (CAD):
- Cause: CAD is often caused by the buildup of atherosclerotic plaques in the coronary arteries. These plaques consist of cholesterol, fat, and other substances that accumulate on the inner walls of the arteries.
- Effect: Over time, the accumulation of plaques can lead to narrowing (stenosis) or blockage of the coronary arteries, reducing blood flow to the heart muscle. This can result in ischemia and structural changes in the heart, especially if the reduced blood supply is chronic or severe.
- Heart Attack (Myocardial Infarction):
- Cause: A heart attack occurs when a coronary artery becomes completely blocked, usually by a blood clot that forms at the site of a ruptured atherosclerotic plaque.
- Effect: The lack of oxygen and nutrients reaching a portion of the heart muscle during a heart attack can cause irreversible damage (infarction) to that area. This damage leads to the formation of scar tissue, altering the structure and function of the heart.
- Valvular Heart Disease:
- Cause: Valvular heart disease can result from various factors, including congenital anomalies, infections, rheumatic fever, and age-related degeneration.
- Effect: Valve stenosis or regurgitation can lead to structural changes in the heart chambers. Stenosis can cause chamber enlargement and increased pressure, while regurgitation can lead to chamber dilation and volume overload.
- Congenital Heart Defects:
- Cause: Congenital heart defects occur due to abnormal development of the heart and its structures during fetal growth.
- Effect: These structural abnormalities can disrupt normal heart function, leading to structural changes that affect blood flow, oxygenation, and chamber size.
- Hypertension (High Blood Pressure):
- Cause: Prolonged, uncontrolled high blood pressure can exert excessive force on the walls of the heart’s chambers and arteries.
- Effect: This pressure overload can lead to hypertrophy (enlargement) of the heart muscle, particularly in the left ventricle. Over time, hypertrophy can result in structural changes and impaired heart function.
- Pericardial Disease:
- Cause: Pericarditis may result from infections, autoimmune conditions, trauma, or other causes. Constrictive pericarditis can develop as a result of chronic inflammation or scarring of the pericardium.
- Effect: Pericardial diseases can restrict the heart’s ability to expand and contract properly, leading to structural limitations and impaired cardiac function.
- Arrhythmogenic Right Ventricular Dysplasia (ARVD):
- Cause: ARVD is a genetic disorder, and its exact cause is related to specific genetic mutations.
- Effect: ARVD can lead to the replacement of heart muscle with fatty or fibrous tissue, affecting both the heart’s structure and its electrical conduction system.
- Cardiac Tumors:
- Cause: The causes of cardiac tumors can vary and may include benign or malignant growths.
- Effect: Tumors can physically occupy space within the heart chambers or the pericardium, potentially obstructing blood flow and causing structural changes.
- Aortic Aneurysm and Dissection:
- Cause: Aortic aneurysms can result from atherosclerosis, genetic factors, or other underlying conditions. Dissections often occur when the inner layer of the aorta tears.
- Effect: These structural issues can disrupt the normal structure of the aorta and impact the heart’s function and blood flow.
It’s important to note that these causes and effects can interact and sometimes lead to a cascade of events that result in complex structural changes in the heart. Early diagnosis, appropriate medical management, and lifestyle modifications are essential for addressing these conditions and minimizing their impact on heart health.
Should I worry about these Structural Changes? Or are they harmless?
Structural changes in the heart should not be ignored, and it’s important to take them seriously because they can have significant implications for your cardiovascular health and overall well-being. While not all structural changes are immediately life-threatening, they can lead to various health issues and complications if left untreated. Here are a few reasons why you should not dismiss structural changes in the heart:
- Progressive Nature: Some structural changes in the heart can progress over time if not addressed. Conditions like hypertension, valvular heart disease, and certain congenital heart defects may worsen if not managed appropriately.
- Risk of Complications: Untreated structural issues can lead to complications such as heart failure, arrhythmias, stroke, or blood clots. These complications can significantly impact your quality of life and overall health.
- Symptoms: Structural changes can cause symptoms like chest pain, shortness of breath, fatigue, palpitations, and edema (swelling). These symptoms can affect your daily activities and should not be ignored.
- Reduced Quality of Life: Structural changes that affect the heart’s ability to pump blood efficiently or maintain normal function can lead to reduced physical capacity, exercise intolerance, and limitations in daily activities.
- Risk of Sudden Events: Some structural issues, such as aortic aneurysms or certain types of cardiomyopathies, can pose a risk of sudden and potentially life-threatening events if they progress or rupture.
- Preventive Measures: Many structural heart issues can be managed effectively with medications, lifestyle changes, and, in some cases, surgical interventions or procedures. Early detection and appropriate treatment can help prevent or delay the progression of these conditions.
- Overall Health: Cardiovascular health is closely linked to overall health. Structural heart problems can increase the risk of other health issues, such as kidney disease, cognitive impairment, and peripheral vascular disease.
It’s important to have regular check-ups with a healthcare provider, especially if you have risk factors for heart disease (e.g., high blood pressure, high cholesterol, smoking, family history of heart disease). If you are diagnosed with a structural heart issue, work closely with your healthcare team to develop a treatment plan and adhere to their recommendations.
While some structural changes may be harmless or benign, only a healthcare professional can determine the nature and severity of the condition. It’s always better to address any concerns or symptoms related to your heart health promptly and seek appropriate medical guidance to ensure the best possible outcome for your cardiovascular health.
How to control these structural changes in the heart?
Controlling and managing structural changes in the heart typically involves a combination of medical treatments, lifestyle modifications, and, in some cases, surgical or interventional procedures. The specific approach depends on the underlying condition and the extent of the structural changes. Here are some general strategies for controlling and managing structural heart issues:
- Medical Treatment:a. Medications: Your healthcare provider may prescribe medications to manage underlying conditions, reduce symptoms, and prevent complications. Common medications include:
- Blood pressure medications (e.g., ACE inhibitors, beta-blockers) for hypertension.
- Diuretics to manage fluid retention.
- Anticoagulants to prevent blood clots.
- Medications to control heart rate and rhythm (e.g., antiarrhythmics).
- Statins to manage cholesterol levels.
- Medications to improve heart function in heart failure (e.g., ACE inhibitors, angiotensin receptor blockers, beta-blockers, diuretics).
- Lifestyle Modifications:a. Diet: Adopt a heart-healthy diet that is low in saturated fats, cholesterol, and sodium. Emphasize fruits, vegetables, whole grains, lean proteins, and unsaturated fats (e.g., olive oil, nuts).b. Exercise: Engage in regular physical activity as recommended by your healthcare provider. Exercise can improve heart health, control blood pressure, and help manage weight.c. Smoking Cessation: Quitting smoking is essential for managing heart conditions. Smoking is a major risk factor for heart disease and can worsen structural heart issues.d. Weight Management: Maintain a healthy weight through a balanced diet and regular physical activity. Obesity can strain the heart and exacerbate structural problems.e. Alcohol: Limit alcohol consumption, as excessive drinking can contribute to heart problems and worsen certain conditions.f. Stress Reduction: Manage stress through relaxation techniques, meditation, mindfulness, or counseling. Chronic stress can impact heart health.g. Medication Adherence: Take prescribed medications as directed by your healthcare provider. Skipping doses or stopping medications can worsen structural heart issues.
- Surgical or Interventional Procedures:a. Angioplasty and Stent Placement: For coronary artery disease, angioplasty with stent placement can open narrowed or blocked arteries and improve blood flow to the heart.b. Valve Repair or Replacement: In cases of severe valvular heart disease, damaged heart valves may need to be repaired or replaced surgically.c. Heart Bypass Surgery (CABG): This procedure can reroute blood flow around blocked coronary arteries to improve blood supply to the heart.d. Aortic Aneurysm Repair: Surgical repair or replacement of an enlarged or dissected aorta may be necessary.e. Cardiac Resynchronization Therapy (CRT): CRT can be used for certain types of heart failure to improve the coordination of the heart’s contractions.f. Implantable Devices: Pacemakers, implantable cardioverter-defibrillators (ICDs), and cardiac resynchronization therapy devices may be recommended to manage arrhythmias and heart failure.
- Regular Medical Follow-Up:a. Schedule and attend regular follow-up appointments with your healthcare provider to monitor the progress of your condition, adjust treatment as needed, and address any concerns or symptoms.
- Cardiac Rehabilitation:a. If recommended, participate in a cardiac rehabilitation program, which provides supervised exercise, education on heart-healthy living, and support for managing heart conditions.
It’s important to work closely with your healthcare team to develop a personalized treatment plan tailored to your specific condition and needs. Adhering to the recommended treatment and lifestyle changes is crucial for managing structural changes in the heart and optimizing your cardiovascular health. Always consult with your healthcare provider for guidance on the most appropriate strategies for your individual situation.
Do I require many drugs for control of these changes, acting on several biochemical pathways?
The number of medications required to control structural changes in the heart depends on several factors, including the specific heart condition you have, the severity of the structural changes, and your individual health status. In some cases, managing heart conditions may involve multiple medications that target different biochemical pathways to achieve optimal control and reduce the risk of complications. Here are some common scenarios where multiple medications may be prescribed:
- Hypertension (High Blood Pressure):
- Controlling high blood pressure may require a combination of medications that work through various mechanisms. This can include ACE inhibitors, beta-blockers, calcium channel blockers, diuretics, and others, depending on your specific needs.
- Coronary Artery Disease (CAD):
- Managing CAD often involves medications to reduce the risk of further plaque buildup and improve blood flow. This can include aspirin, statins to lower cholesterol, antiplatelet drugs, beta-blockers, and nitroglycerin.
- Heart Failure:
- Heart failure management typically includes a combination of medications to reduce symptoms and improve heart function. This can include ACE inhibitors or angiotensin receptor blockers (ARBs), beta-blockers, diuretics, and, in some cases, medications like sacubitril/valsartan (ARNI) or aldosterone antagonists.
- Valvular Heart Disease:
- Medications may be prescribed to manage symptoms and reduce complications associated with valvular heart disease. For example, diuretics may help with fluid retention, and medications to control blood pressure or heart rate may be necessary.
- Arrhythmias:
- Depending on the type of arrhythmia, antiarrhythmic medications may be prescribed to control heart rhythm. Additionally, medications to reduce the risk of blood clots (anticoagulants) may be necessary for certain arrhythmias like atrial fibrillation.
- Prevention of Blood Clots:
- Some structural heart issues, such as atrial fibrillation or artificial heart valves, require anticoagulant medications (e.g., warfarin or newer direct oral anticoagulants) to prevent the formation of blood clots that could lead to strokes or other complications.
- Secondary Conditions:
- In addition to specific heart-related medications, you may also need medications to manage other health conditions that can impact your cardiovascular health, such as diabetes, high cholesterol, or kidney disease.
- Symptom Relief:
- Medications may be prescribed to alleviate symptoms associated with heart conditions, such as pain relief for angina or shortness of breath in heart failure.
While taking multiple medications may be necessary to effectively manage heart conditions and control structural changes, it’s essential to work closely with your healthcare provider to ensure that the medications are appropriate for your specific situation. Your healthcare team will carefully consider the potential benefits, risks, and interactions of these medications to develop a treatment plan that optimizes your cardiovascular health while minimizing side effects.
Additionally, regular follow-up appointments with your healthcare provider are important to monitor your response to the medications and make any necessary adjustments to your treatment plan. Adherence to prescribed medications and lifestyle changes is crucial for effectively managing structural heart issues and improving overall heart health.