Excerpt
Heart failure, a chronic condition where the heart can’t pump blood efficiently, is a major health concern, particularly in India. It’s characterized by reduced pumping and relaxing efficiency of the heart, leading to symptoms like fatigue, shortness of breath, and fluid retention. Heart failure can manifest as reduced ejection fraction (HFrEF) or preserved ejection fraction (HFpEF), each with distinct causes and treatments. Regular monitoring and management are crucial for improving patients’ quality of life and longevity. Early detection and intervention can prevent heart failure from advancing to more severe stages, highlighting the importance of understanding and addressing this condition proactively.
Introduction
Heart failure, a chronic and progressive condition where the heart muscle is unable to pump enough blood to meet the body’s needs, is a significant public health concern worldwide, particularly so, in India.
Heart Failure (aka congestive heart failure) affects millions of people, leading to substantial morbidity, mortality, and health care costs.
Despite its name, heart failure does not mean the heart has stopped working; rather, it signifies a reduced efficiency in its dynamically powered pumping and relaxing functions.
This inefficiency can lead to a host of symptoms, impacting patients’ quality of life and longevity.
1. Understanding Heart Failure
Types of Heart Failure (aka congestive heart failure)
1. Heart Failure with Reduced Ejection Fraction (HFrEF): Also known as systolic heart failure, HFrEF occurs when the heart muscle becomes weak and cannot contract effectively.
The ejection fraction, a measurement of the percentage of blood leaving the heart each time it contracts, is significantly reduced in congestive heart failure with reduced ejection fraction (<50%). This type of heart failure is often a result of conditions that damage the heart muscle, such as coronary artery disease, heart attack, or cardiomyopathy.
Heart Failure with Preserved Ejection Fraction (HFpEF): In heart failure with preserved ejection fraction, also known as diastolic heart failure, the heart muscle becomes stiff and does not relax properly between beats. This stiffness limits the heart’s ability to fill with blood, resulting in inadequate blood flow to the rest of the body.
Heart failure with preserved ejection fraction is often associated with hypertension, diabetes, and obesity. Unlike Heart failure with reduced ejection fraction, the ejection fraction in Heart failure with preserved ejection fraction may remain normal (=>50%), but the heart’s inability to relax properly is a key problem, you need to understand..
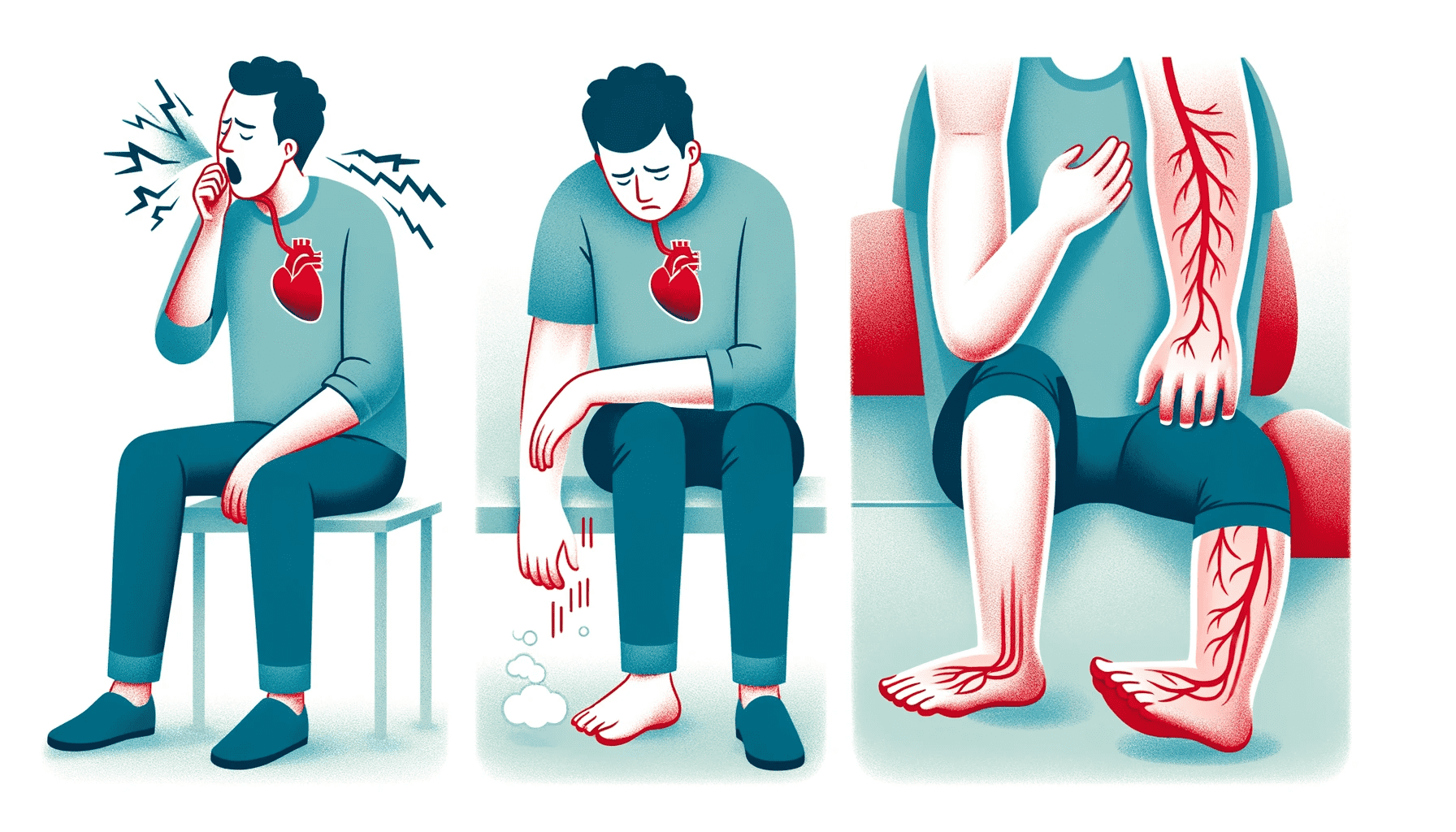
Common Symptoms of Heart Failure
Heart failure symptoms can vary depending on the type and severity of the condition, but some common symptoms include:-
Fatigue: Patients often feel tired easily, as your body tissues and organs do not receive enough oxygen-rich blood.
Shortness of Breath (dyspnea) can occur during activity, while at rest, or even while lying flat. This symptom is due to fluid build-up in the lungs, making breathing difficult.
Fluid Retention: Manifests as swelling (edema), particularly in the legs, ankles, and abdomen. Fluid retention is a result of the heart’s reduced pumping action, causing fluid to back up in the tissues.
Others: Symptoms include rapid or irregular heartbeat, reduced ability to exercise, persistent cough or wheezing, increased urination at night, and swelling of the abdomen.
2. Symptoms and Early Warning Signs
Recognizing the symptoms and early warning signs of heart failure in heart failure clinic is critical for timely diagnosis and effective management.
Heart failure can present a variety of symptoms, which may vary in severity and can fluctuate over time.
Common symptoms include leg swelling, difficulty in breathing, chest pain, and palpitations, each of which signals different aspects of the heart’s declining function.
Leg Swelling (Edema)
Cause: In heart failure, the heart’s reduced capacity to pump blood effectively leads to fluid accumulation in the body’s tissues, most notably in the lower extremities. This is known as peripheral edema.
Appearance: Swelling is often noticeable in the feet, ankles, and legs, but it can also occur in the abdomen and other parts of the body.
Monitoring: Monitoring the extent of swelling and any changes in its severity can provide important clues about the progression of heart failure.
Difficulty in Breathing (Dyspnea)
Cause: Fluid accumulation in the lungs, known as pulmonary edema, is a common consequence of Heart failure. This can make it difficult for patients to breathe, especially during physical activity or when lying flat.
Symptoms: Patients may experience shortness of breath, a feeling of being suffocated, or a need to prop themselves up with pillows to breathe easier at night (orthopnea).
Orthopnoea is a special type, where patient becomes breathless after some time of lying down flat.
Trepopnoea occurs while the patient is recumbent, turning to left or right side produces dyspnoea.
Difficulty in breathing is often the symptom in heart failure clinic that frequently leads to seeking medical attention.
Chest Pain
- Nature: Chest pain in heart failure arises from the heart struggling to function under increased stress or may be a sign of co-existing coronary artery disease.
- Attention: Any new or worsening chest pain should be evaluated promptly, as it can also be a sign of a heart attack.
Palpitations
- Experience: Palpitations, or the sensation of having a fast-beating, fluttering, or pounding heart, can occur due to the heart’s attempt to compensate for its reduced pumping capacity.
- Related Arrhythmias: Heart failure can lead to arrhythmias (irregular heartbeats), which might manifest as palpitations in a heart failure clinic.
Other Early Warning Signs
- Increased Fatigue: Feeling unusually tired or weak during everyday activities is an early sign of heart failure.
- Weight Gain: Sudden weight gain may indicate fluid retention, a common occurrence in heart failure.
- Decreased Appetite and Nausea: As fluid accumulates in the digestive tract, it can cause feelings of fullness, decreased appetite, or nausea.
- Cognitive Changes: Confusion or impaired thinking can occur, often due to reduced blood flow to the brain.Early Detection in heart failure clinic
Heart failure, a progressive condition in which the heart’s ability to pump blood efficiently becomes impaired. When symptoms are detected and managed early, healthcare providers can implement treatment strategies that may prevent the disease from advancing to more severe stages. This can help preserve heart function and reduce the risk of complications.
- Enhancing Quality of Life: Heart failure symptoms, such as shortness of breath, fatigue, and fluid retention, can significantly impact a person’s daily life and activities. Early intervention can alleviate these symptoms, leading to an improved quality of life. Patients may find it easier to perform daily tasks and enjoy a higher level of physical comfort and well-being.
- Reducing Hospitalizations: Untreated or poorly managed heart failure often leads to recurrent hospitalizations. Early detection allows healthcare professionals to initiate appropriate treatments and monitor the patient’s condition closely. This proactive approach can reduce the frequency and duration of hospital stays, minimizing the physical and emotional toll on patients and their families.
- Optimizing Treatment Strategies: When heart failure is detected early, healthcare providers have a wider range of treatment options at their disposal. Medication adjustments, lifestyle modifications (such as dietary changes and exercise programs), and other interventions can be implemented to address the specific needs and challenges of each patient. These tailored approaches can lead to more effective management of the condition.
- Preventing Complications: Heart failure is associated with several potential complications, including arrhythmias, kidney problems, and heart valve issues. Early detection allows healthcare professionals to identify and address these complications before they become more severe, reducing
the overall health risks for the patient.
5. Early detection and management of heart failure symptoms are fundamental to improving the prognosis and quality of life for individuals living with this condition in a heart failure clinic. It is a collaborative effort between patients and healthcare providers that can ultimately lead to better outcomes and a more positive experience for those affected by heart failure.
Early signs and symptoms
Understanding and recognizing the symptoms and early warning signs are important in heart failure clinic.
It allows patients and heart failure clinics to take timely action, optimizing treatment strategies and potentially slowing the progression of heart failure.
This proactive approach is a key component in the effective management of heart failure in a heart failure clinic, underscoring the importance of patient education and awareness.
3. Dietary Considerations
Diet plays a crucial role in managing congestive heart failure (CHF), a condition where the heart is unable to pump blood efficiently.
Patients with heart failure often struggle with fluid retention, which can exacerbate their symptoms and worsen their condition.
Therefore, dietary modifications you need to make are a key component of heart failure management, aimed at preventing fluid overload and maintaining optimal nutritional status.
Limiting Salt and Fluid Intake
- Salt Restriction: Sodium is a key factor in fluid retention. Patients with heart failure are advised to limit their salt intake to less than 2,000 milligrams per day. High-sodium foods such as processed meats, canned soups, fast foods, and salty snacks should be avoided in your food.
- Fluid Intake: While hydration is important for overall health, excessive fluid intake leads to a dangerous accumulation in heart failure.
- Fluid intake can vary, but generally, patients are advised to limit fluid intake to about 1.5 – 2 liters per day, depending on their condition.
- Reading Labels: Understanding food labels is vital for heart failure patients to monitor their sodium and fluid intake effectively.
Emphasizing a Balanced Diet
- Fruits and Vegetables: These are high in vitamins, minerals, and fiber, and low in calories and sodium. They should form a significant part of the diet. When treatment is initiated, attention on certain parameters like Serum Potassium is crucial.
- Whole Grains: Foods like brown rice, whole wheat bread, and oatmeal provide necessary fiber without the added sodium present in many processed grains.
- Lean Proteins: Sources like fish, skinless poultry, beans, and legumes provide essential nutrients without the harmful fats and sodium found in processed meats.
- Low-Fat Dairy Products: These can provide calcium and protein without excessive salt or saturated fats.
Foods to Avoid
- High-Salt Foods: Salted nuts, chips, pickles, cheese, and deli meats are high in sodium and should be limited.
- Saturated and Trans Fats: These fats, found in fried foods, baked goods, and fatty meats, can increase the risk of heart disease.
- Sugar: Excessive sugar intake can lead to weight gain and worsen heart failure symptoms. Patients should limit sugary drinks, candies, and desserts.
Nutritional Monitoring
- Regular Weighing: Regular weighing helps monitor fluid retention, an important aspect of managing heart failure in a heart failure clinic.
- Consulting a Dietitian: A dietitian in the heart failure clinic can provide personalized advice and meal plans to meet individual nutritional needs and preferences.
The Role of Supplements
- Potassium and Magnesium: Certain heart failure medications can deplete potassium and magnesium. These minerals are important for heart health and may need to be supplemented, but only under medical supervision.
- Omega-3 Fatty Acids: Found in fish oil, they may benefit heart health. However, patients should consult with their healthcare provider before starting any supplements.

Dietary management in heart failure is not just about restricting certain foods but also about maintaining a balanced, nutritious diet that supports overall health and well-being.
Proper dietary habits can significantly impact the severity of symptoms and the progression of heart failure.
Patients with heart failure should work closely with their healthcare team, including dietitians, to develop and adhere to dietary plans tailored to their specific needs and health goals.
4. Treatment Options for Heart Failure
The treatment of heart failure in a heart failure clinic is multifaceted and depends significantly on the type of heart failure – HFrEF (Heart Failure with Reduced Ejection Fraction) or HFpEF (Heart Failure with Preserved Ejection Fraction).
While there are common strategies in managing both types, specific treatments may vary, focusing on alleviating symptoms, preventing disease progression, and improving quality of life.
Treatment for HFrEF
- ACE Inhibitors: These medications help relax blood vessels, lower blood pressure, and reduce the heart’s workload. Examples include ramipril, lisinopril and enalapril.
- Beta-Blockers: They slow the heart rate and reduce blood pressure. Carvedilol, bisoprolol and metoprolol are commonly used beta-blockers in HFrEF treatment.
- Diuretics: Often referred to as water pills, diuretics help reduce fluid accumulation in the body, alleviating symptoms such as swelling and shortness of breath. Furosemide is a widely used diuretic.
- Aldosterone Antagonists: Spironolactone, Eplerenone and Finerenone can be used to reduce fluid retention and have been shown to improve survival in HFrEF.
- ARNI (Angiotensin Receptor-Neprilysin Inhibitors): A newer class of drugs, such as sacubitril valsartan, that combines an angiotensin receptor blocker with a neprilysin inhibitor, showing promising results in reducing heart failure symptoms and improving survival. (Click here for technical article)
- Vericiguat: A recently developed novel oral soluble guanylate cyclase stimulator, vericiguat, in patients with HFrEF is promising.
- Digitalis: This medication can strengthen heart muscle contractions and may be used to control the heart rate.
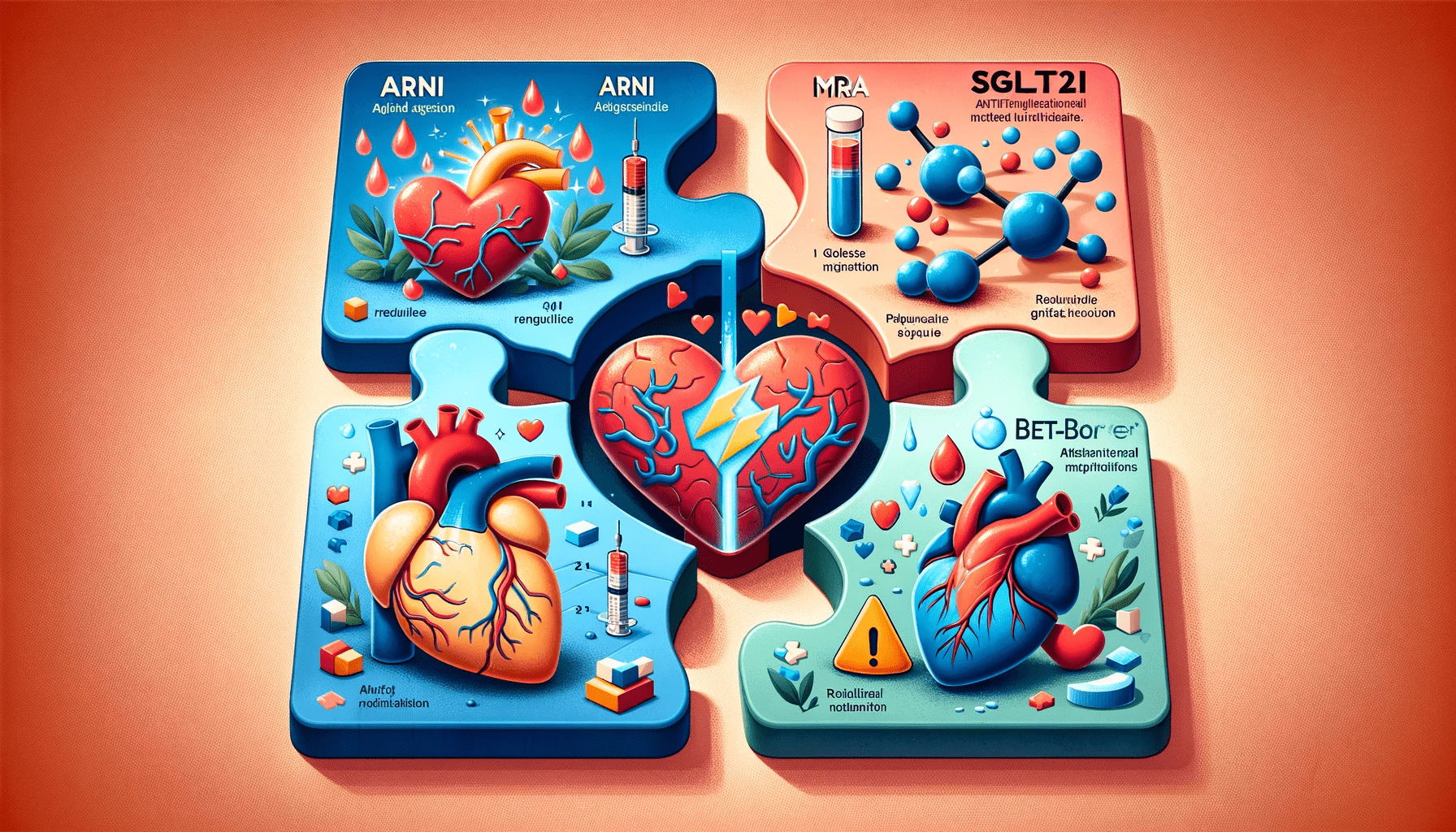
Treatment for HFpEF
- Managing Comorbidities: Key to treating HFpEF is the management of underlying conditions such as hypertension, diabetes, and obesity.
- Diuretics: Similar to HFrEF, diuretics are used to manage fluid retention.
- SGLT2 inhibitors: Medications like Dapagliflozin, Empagliflozin
- Blood Pressure Control: Medications like ACE inhibitors, ARBs (Angiotensin II Receptor Blockers), and beta-blockers may be used to control high blood pressure.
- Heart Rate Management: Medications such as beta-blockers, ivabradine and calcium channel blockers can be used to manage heart rate and improve heart filling.
Emphasis on Individualized Care
- Tailored Treatment: Recognizing that heart failure manifests differently in each individual, treatments are increasingly tailored in every heart failure clinic to the specific needs and characteristics of the patient.
- Multidisciplinary Approach: Involvement of cardiologists, primary care physicians, dietitians, and other specialists to address all aspects of the patient’s health in a heart failure clinic.
- Integration of Recent Guidelines
- Updated Protocols: Treatment protocols are continually updated to incorporate the latest research findings and recommendations from leading medical organizations.
- Novel Medications: The introduction of new medications and therapies based on the latest clinical trials and studies.
The treatment of heart failure is complex and evolving.
It requires a comprehensive approach that combines medication, lifestyle changes, and possibly surgical interventions. Regular follow-ups and adjustments in treatment strategies are crucial for managing heart failure in heart failure clinic effectively.
As research advances, treatment protocols continue to evolve, offering hope for improved outcomes and quality of life for patients with heart failure.
5. Living with Heart Failure and Quality of Life (QOL)
Living with heart failure presents numerous challenges, but with the right approach, patients can manage their condition effectively and maintain a good quality of life.
The key to successful management in heart failure clinic lies in embracing lifestyle changes, adhering to treatment plans, and being proactive about health monitoring.
Lifestyle Modifications
- Regular Exercise: Physical activity is crucial in managing heart failure. It strengthens the heart muscle, improves circulation, and aids in maintaining a healthy weight.
- Exercise routines should be tailored to individual capabilities and medical advice.
- Activities like walking, swimming, or light aerobic exercises can be beneficial.
- Dietary Changes: A heart-healthy diet low in sodium, saturated fats, and added sugars, and rich in fruits, vegetables, and whole grains is essential. Portion control and regular meal times also help in managing weight and overall health.
- Quitting Smoking: Smoking cessation is critical as it significantly reduces the risk of further heart damage and other complications. There are various support programs and medications that can assist in quitting smoking.
- Limiting Alcohol and Caffeine: Both alcohol and caffeine can have adverse effects on heart health and should be consumed in moderation or avoided entirely, based on medical advice.
- Stress Management: Chronic stress can exacerbate heart failure symptoms. Techniques such as meditation, yoga, deep breathing exercises, or counseling can be effective in managing stress.
Active Health Management
- Symptom Monitoring: Regular monitoring of symptoms like weight gain, swelling, shortness of breath, or fatigue is vital. Sudden changes in these symptoms may indicate a need for medical attention.
- Medication Adherence: Adhering to prescribed medication regimens is critical in managing heart failure. Patients should understand their medications, their purposes, and the importance of taking them as directed.
- Regular Medical Check-ups: Routine follow-ups with healthcare providers help in monitoring the condition, making necessary adjustments in treatment, and addressing any concerns.
- Self-Care Education: Understanding the condition, its triggers, and management strategies empowers patients to take an active role in their care.
Psychosocial Aspects
- Social Support: Engaging with family, friends, and support groups can provide emotional and practical support. Sharing experiences with others in similar situations can be particularly comforting and informative.
- Mental Health: The psychological impact of living with a chronic condition like heart failure cannot be overlooked. Depression and anxiety are common and should be addressed with professional help.
- Quality of Life (QOL): Enhancing QOL involves balancing medical needs with everyday living. It’s about making adjustments to live as fully as possible despite the limitations imposed by heart failure.
6. Prognosis and Life Expectancy
The prognosis for patients with heart failure has seen considerable improvement over the years, thanks largely to advancements in medical treatment, better understanding of the disease, and more effective management strategies.
However, life expectancy in heart failure patients varies widely and is influenced by several factors.
Factors Influencing Prognosis and Life Expectancy
- Age: Younger patients often have a better prognosis, partly because they typically have fewer comorbid conditions and a better ability to tolerate aggressive treatments.
- Severity of the Condition: The stage of heart failure significantly impacts prognosis. Patients with advanced heart failure (e.g., those who experience symptoms at rest) generally have a poorer prognosis compared to those in earlier stages.
- Comorbid Conditions: The presence of other medical conditions like diabetes, kidney disease, or chronic obstructive pulmonary disease can complicate heart failure management and affect prognosis.
- Treatment Adherence: Regularly taking prescribed medications, following dietary recommendations, and attending medical appointments are crucial for managing heart failure effectively and improving life expectancy.
- Lifestyle Factors: Smoking, physical inactivity, and poor diet can worsen heart failure and negatively impact prognosis.
- Response to Treatment: How well a patient responds to heart failure
treatment can also influence their prognosis.
Improvements in Treatment and Management
- Medication Advances: The development of new classes of medications, like ARNI, and improvements in existing therapies have significantly improved outcomes in heart failure patients.
- Device Therapy: The use of devices such as pacemakers and defibrillators has been shown to improve survival in certain groups of heart failure patients.
- Heart Transplantation and Left Ventricular Assist Devices (LVADs): For patients with advanced heart failure, these interventions can be life-saving.
7. Innovations and Future Directions in Heart Failure Treatment
The landscape of heart failure treatment is continuously evolving, driven by groundbreaking research and technological advancements. Recent years have seen significant strides in developing new medications, refining existing therapies, and enhancing our understanding of heart failure mechanisms.
These innovations not only promise better management of the condition but also open doors to potentially curative treatments in the future.