
- Beneath the Sun’s relentless, scorching glare,
A weary horse trudges, burdened by despair.
Blind to its fatigue Its rider demands speeds,
Unaware that rest is what the beast truly needs. - On the brink of collapse, with every step it takes,
Only a respite, a meal, a dream, its spirit awakes.
Let it lie down, under the shade, in peace to sleep,
To rise with dawn, rejuvenated, no promises to keep.
Introduction
Heart failure, a critical public health issue, is increasingly recognized for its substantial impact on global morbidity and mortality rates. Characterized by the heart’s inability to pump blood sufficiently to meet the body’s needs, heart failure affects approximately 26 million individuals worldwide, making it a leading cause of hospitalization for heart failure (HFH) among adults over the age of 65. The condition significantly impairs quality of life, leading to recurrent hospitalizations, diminished physical capacity, and a heightened risk of premature death.

Definition and significance
The clinical syndrome of heart failure results from any structural or functional cardiac disorder that impairs the ventricle’s ability to fill with or eject blood. The importance of heart failure in cardiology cannot be overstated, as it sits at the intersection of various cardiovascular diseases, including hypertensive heart disease, coronary artery disease, and valvular heart disease. Its development is often the culmination of the progressive worsening of any of these conditions, making its management a complex and multifaceted challenge in cardiovascular care.

Heart failure’s significance extends beyond the individual, exerting a considerable burden on healthcare systems worldwide due to the high costs associated with long-term treatment, management of acute decompensation events, and hospital readmissions. The condition’s prevalence is on the rise, attributed to aging populations and increasing survival rates from other cardiovascular conditions, thereby amplifying its impact on public health and underscoring the urgent need for effective management strategies and therapeutic interventions in the field of cardiology.
The Etiology
The etiology of heart failure is multifactorial, encompassing both genetic and acquired factors. Ischemic heart disease, precipitated by atherosclerotic coronary artery disease, is a predominant cause, leading to myocardial infarction and subsequent loss of contractile tissue. Cardiomyopathies, which include dilated, hypertrophic, and restrictive forms, directly impair myocardial structure and function.

Valvular heart diseases, such as aortic stenosis and mitral regurgitation, impose abnormal hemodynamic stresses on the heart, while systemic conditions like hypertension and diabetes mellitus induce pathological changes through mechanisms like pressure overload and glycotoxicity, respectively. These diverse etiologies contribute to the complex pathobiology of heart failure, necessitating a comprehensive understanding for effective management.
The Pathophysiology
The pathophysiology of heart failure is complex, underpinned by a spectrum of mechanisms leading to the heart’s compromised efficacy in blood circulation. This dysfunction can be categorized into two primary forms: systolic and diastolic. Systolic dysfunction, or heart failure with reduced ejection fraction (HFrEF), is characterized by the heart’s diminished contractile power, resulting in a decreased ejection fraction. This impairment in myocardial contractility often stems from ventricular remodeling, a consequence of chronic hemodynamic overload or ischemic myocardial damage, leading to dilatation and spherical deformation of the ventricular chamber.
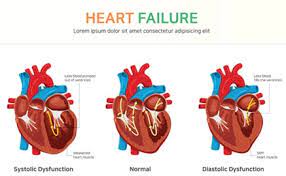
Diastolic dysfunction, or heart failure with preserved ejection fraction (HFpEF), involves the heart’s inability to relax and fill adequately during diastole, despite a normal ejection fraction. This condition is frequently associated with myocardial hypertrophy and fibrosis, which elevate ventricular stiffness, impeding proper ventricular filling due to increased end-diastolic pressures.
Classification of Heart Failure
The classification of heart failure (HF) into heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF) is pivotal in the realm of cardiology, serving as a foundation for delineating pathophysiological distinctions and guiding therapeutic interventions. HFrEF is identified when the left ventricular ejection fraction (LVEF) is less than 40%, indicating a primary deficit in myocardial contractility. This condition is often the sequelae of coronary artery disease, leading to systolic dysfunction. Conversely, HFpEF, defined by an LVEF of 50% or greater, is characterized by normal systolic function but impaired diastolic filling due to increased ventricular stiffness or abnormal relaxation, frequently associated with hypertension and myocardial hypertrophy.
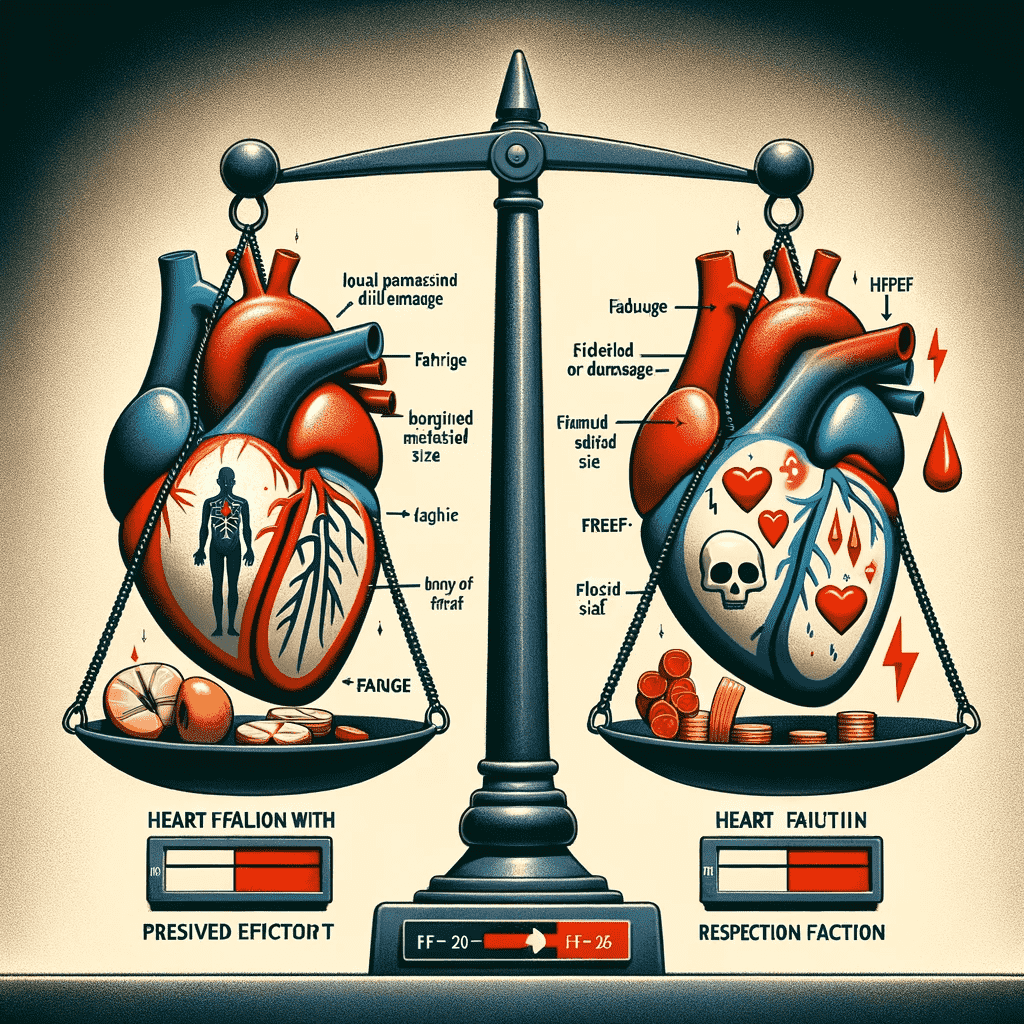
The clinical significance of distinguishing between HFrEF and HFpEF lies in their divergent therapeutic pathways; HFrEF benefits from evidence-based therapies such as ACE inhibitors, beta-blockers, and mineralocorticoid receptor antagonists, which have been shown to improve survival, whereas HFpEF management focuses on controlling comorbid conditions and symptoms, with fewer evidence-based treatment options available.
Heart failure is also stratified into stages A through D by the American Heart Association and American College of Cardiology (AHA/ACC), reflecting the progression from risk of HF to advanced heart disease. Stage A encompasses individuals at risk of HF without structural heart disease or symptoms, progressing to Stage D, which represents refractory HF requiring specialized interventions.

This staging system is crucial for prognostication and tailoring patient management, highlighting the disease’s progressive nature and the escalating intensity of treatment required as HF advances. Understanding these classifications and stages aids in optimizing patient outcomes through early intervention and appropriate, stage-specific management strategies.
Therapeutic strategies in HF management
Pharmacological interventions form the cornerstone of heart failure (HF) management, targeting the underlying pathophysiological mechanisms to ameliorate symptoms, enhance quality of life, and improve prognosis. Beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), angiotensin receptor/neprilysin inhibitor, is made up of two drugs put together to treat heart failure (ARNI). It contains an ARB (angiotensin II receptor blocker) and a neprilysin and diuretics are integral to this therapeutic arsenal, each with distinct mechanisms of action and clinical benefits.

Beta-blockers mitigate the deleterious effects of sympathetic nervous system overactivity on the heart by blocking beta-adrenergic receptors, thereby reducing heart rate, myocardial oxygen demand, and arrhythmic risks. This class of medication has been shown to improve survival rates in patients with HFrEF by attenuating adverse cardiac remodeling.
ACE inhibitors and ARBs act on the renin-angiotensin-aldosterone system (RAAS), a pivotal regulatory axis in cardiovascular homeostasis. ACE inhibitors prevent the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor and stimulator of aldosterone secretion, thereby reducing preload and afterload, and diminishing the progression of ventricular remodeling. ARBs selectively block angiotensin II receptors, offering a similar spectrum of hemodynamic and prognostic benefits, particularly in patients intolerant to ACE inhibitors.
Diuretics, including loop, thiazide, and potassium-sparing varieties, play a crucial role in managing fluid overload, a hallmark of HF. By promoting sodium and water excretion, they alleviate pulmonary and peripheral edema, thereby improving dyspnea and exercise tolerance.
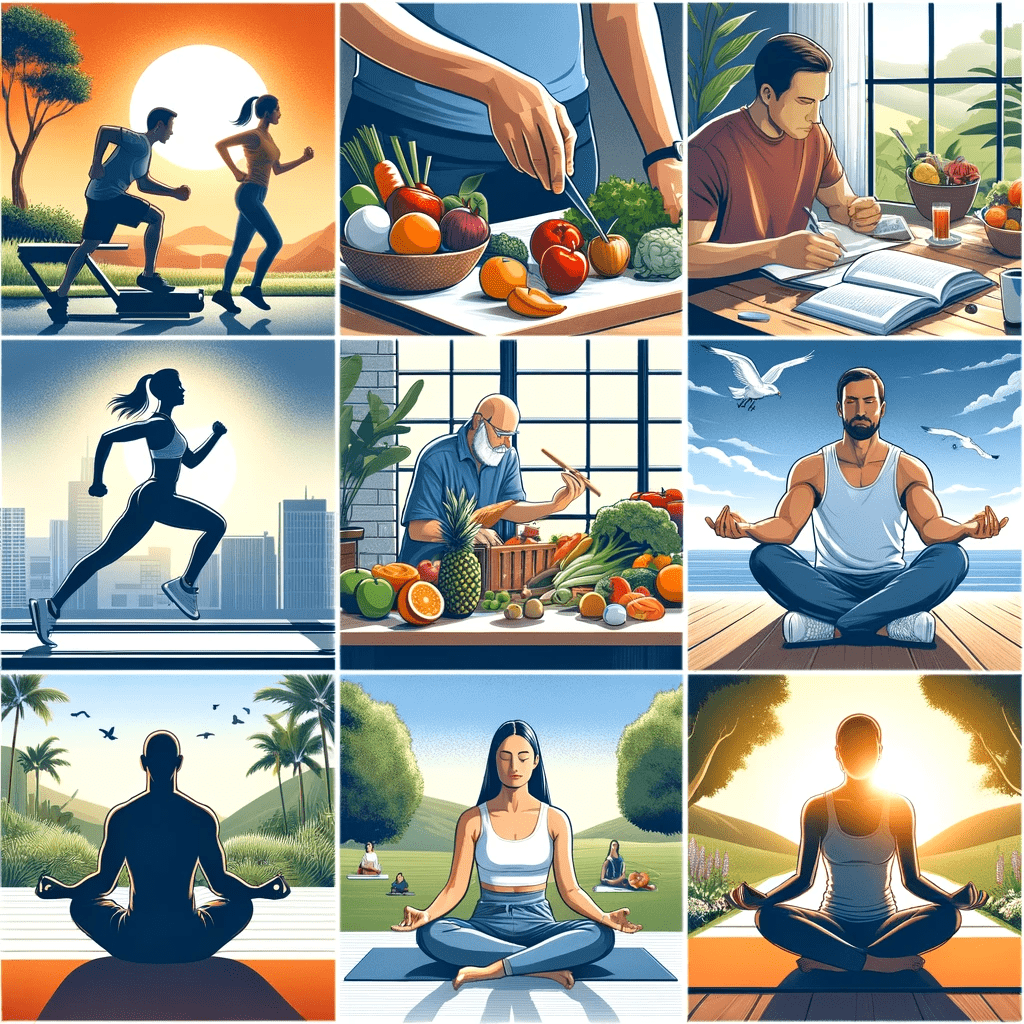
Beyond pharmacotherapy, lifestyle modifications and non-pharmacological approaches are vital in managing HF. Dietary sodium restriction, fluid management, regular physical activity, and weight reduction in overweight patients are recommended to control symptoms and prevent hospitalizations. Smoking cessation and alcohol moderation are also advised to mitigate cardiovascular risk factors. Collectively, these interventions underscore a holistic strategy in HF management, emphasizing the synergy between pharmacological and non-pharmacological measures in optimizing patient outcomes.
Advanced therapies and surgical management
Advanced therapies and surgical interventions are pivotal in the management of heart failure (HF), particularly for patients with refractory symptoms or end-stage disease. Device-based therapies, including implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT), have revolutionized the treatment landscape, offering significant mortality benefits and symptom improvement.
ICDs are sophisticated devices designed to continuously monitor heart rhythms and deliver life-saving shocks or pacing therapy in response to detected ventricular arrhythmias, which are common in HF and can be fatal. The primary role of ICDs is in the secondary prevention of sudden cardiac death among patients with a history of life-threatening arrhythmias and in the primary prevention for specific populations at high risk, as delineated by evidence-based guidelines.
CRT devices, on the other hand, address cardiac dyssynchrony—a condition where the heart’s ventricles contract in an uncoordinated manner, common in advanced HF. By simultaneously pacing both the left and right ventricles, CRT improves the efficiency of the heart’s contractions, enhancing ejection fraction, reducing HF symptoms, and improving survival. CRT is indicated for patients with symptomatic HF despite optimal medical therapy, who have a widened QRS complex on electrocardiogram indicative of dyssynchrony.
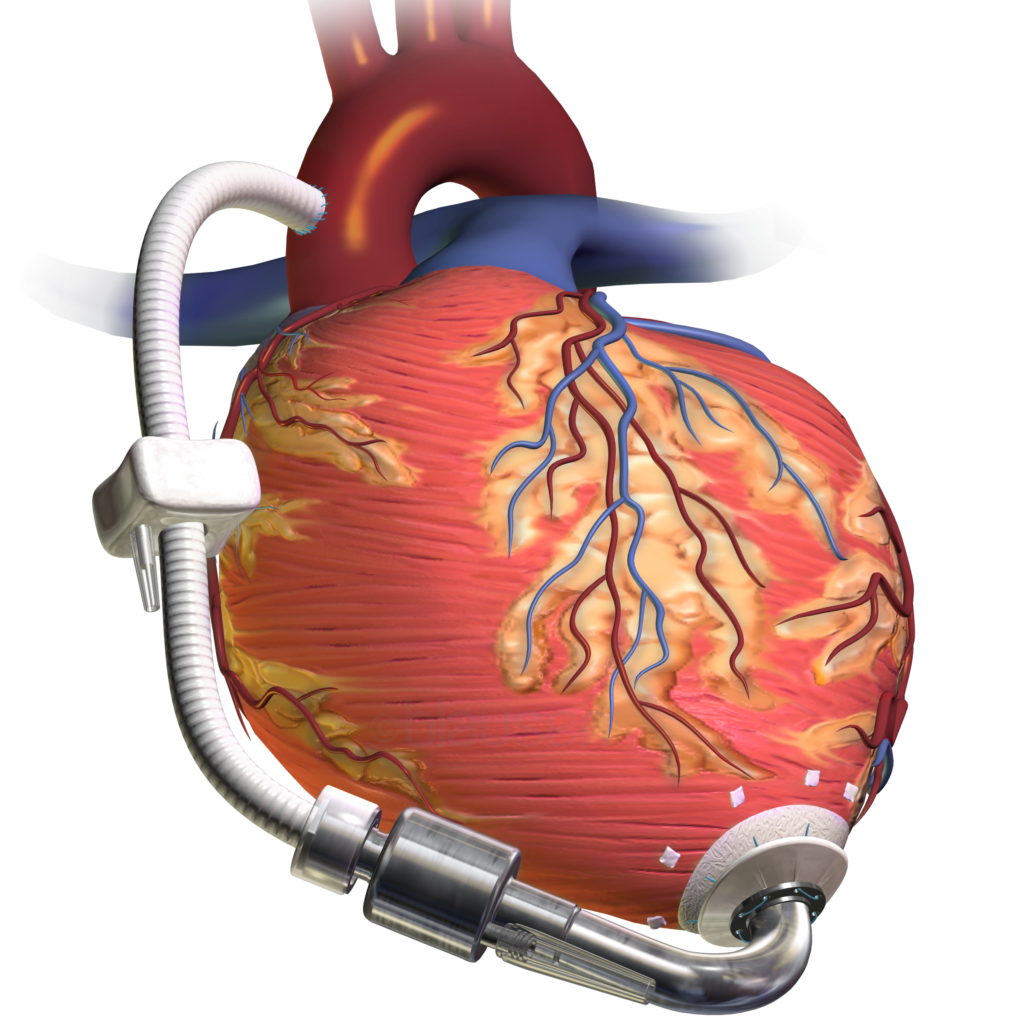
For patients with advanced HF refractory to medical and device therapy, surgical options such as ventricular assist devices (LVADs, pronounced elvaadhs) and heart transplantation represent the pinnacle of intervention. LVADs are mechanical pumps that support or replace the function of a failing heart, either as a bridge to transplantation or as destination therapy. Heart transplantation remains the definitive treatment for end-stage HF, offering the potential for a significantly improved quality of life and survival, albeit limited by donor availability and the need for lifelong immunosuppression. These advanced therapeutic modalities underscore the importance of a multidisciplinary approach in managing complex HF cases, integrating cutting-edge technology and surgical expertise to extend and enhance patient lives.
Emerging trends in HF management

Emerging trends in heart failure (HF) treatment have significantly shifted the therapeutic paradigm, particularly with the advent of novel pharmacological agents and the integration of precision medicine. Sacubitril/valsartan, a landmark agent in this arena, exemplifies these advances. As a first-in-class angiotensin receptor-neprilysin inhibitor (ARNI), it synergistically enhances the protective neurohormonal systems while suppressing the deleterious ones. By inhibiting neprilysin—an enzyme that degrades natriuretic peptides—and blocking angiotensin II receptors, sacubitril/valsartan facilitates vasodilation, natriuresis, and inhibition of fibrosis and hypertrophy. Clinical trials, notably the PARADIGM-HF trial, have demonstrated its superiority over enalapril in reducing mortality and hospitalization rates in patients with HFrEF, marking a significant leap in HF management.

Parallelly, precision medicine in HF is harnessing genomic insights and biomarker-driven strategies to tailor treatments to individual patient profiles. This approach involves identifying genetic variants and biomarkers that predict response to therapies, disease progression, and prognosis. For instance, genetic polymorphisms affecting beta-adrenergic signaling pathways can influence responses to beta-blocker therapy in HF. Similarly, biomarkers like natriuretic peptides and troponins are integral to diagnosing HF severity and guiding treatment intensity. This shift towards a more nuanced, patient-specific approach promises to optimize therapeutic outcomes, minimize adverse effects, and usher in a new era of personalized HF care.
Challenges and Opportunities in Heart Failure Management
Managing heart failure (HF) presents a complex array of challenges for patients and healthcare providers alike, stemming from the disease’s chronic nature, the need for lifelong management, and the intricacies of its treatment. Barriers to optimal care include medication adherence issues, access to specialized care, and the management of comorbid conditions, which can complicate treatment and exacerbate symptoms. Additionally, healthcare systems face challenges in providing multidisciplinary care and ensuring continuity of care across transitions from hospital to home.
Looking towards the future, heart failure treatment is poised for transformative changes driven by advancements in technology, pharmacology, and a deeper understanding of the disease’s molecular basis. Innovations in remote patient monitoring and telehealth promise to enhance patient management, enabling real-time adjustments to treatment regimens and reducing hospital readmissions. In pharmacology, the development of novel agents that target the underlying molecular mechanisms of HF more precisely is anticipated, potentially offering improved efficacy and reduced side effects. Furthermore, the burgeoning field of regenerative medicine, including stem cell therapy and tissue engineering, holds the promise of repairing or replacing damaged cardiac tissue. As research continues to unravel the genetic underpinnings of HF, personalized medicine approaches are expected to refine treatment strategies, making them more effective and individualized. Together, these advancements herald a hopeful future for heart failure management, characterized by improved outcomes and quality of life for patients.
Patient-Centered Care in Heart Failure
Patient-centered care is paramount in managing heart failure (HF), with patient education and the integration of patient preferences at its core. Educating patients about their condition, treatment options, and lifestyle modifications is critical for empowering them to actively participate in their care. Understanding the complexities of HF, including symptom monitoring, medication adherence, and recognizing warning signs of exacerbation, enables patients to better manage their condition and seek timely medical intervention. This informed engagement can lead to improved outcomes, reduced hospitalizations, and a higher quality of life.

Incorporating patient preferences into treatment planning is equally vital. HF is a multifaceted condition that impacts patients’ lives in diverse ways, making personalized care strategies essential. Discussions about treatment goals should consider patients’ values, lifestyle preferences, and their willingness to accept potential trade-offs associated with different therapies. For instance, some patients may prioritize medication regimens that minimize side effects over those that might offer marginal improvements in survival but significantly impact daily living. Engaging patients in shared decision-making respects their autonomy and aligns treatment plans with their individual goals and quality of life expectations, fostering adherence and satisfaction with care. This patient-centered approach is a cornerstone of effective HF management, ensuring that treatment strategies are both clinically effective and personally meaningful.
The future of HFrEF management
Looking forward, the future of HF management is bright, with ongoing research and innovation poised to revolutionize care. Advancements in genomics, biomarker identification, and regenerative medicine, including stem cell therapy and tissue engineering, hold the promise of addressing the fundamental causes of HF.

Additionally, the evolution of telehealth and remote monitoring technologies is set to enhance patient engagement and adherence, providing real-time adjustments to treatment regimens. Together, these advancements herald a new era in HF management, where personalized, effective, and holistic strategies will significantly improve patient outcomes, offering hope to millions affected by this condition.
Conclusion
In conclusion, the management of heart failure (HF) encompasses a comprehensive approach that integrates pharmacological interventions, lifestyle modifications, advanced therapies, and patient-centered care. Pharmacological treatments, including beta-blockers, ACE inhibitors, ARBs, and diuretics, alongside novel agents like sacubitril/valsartan, form the backbone of therapy, targeting the underlying pathophysiological mechanisms to improve survival and quality of life.

The importance of lifestyle changes and the inclusion of device-based therapies, effectiveness of EECP non-interventional therapy and surgical options further underscore the multifaceted nature of HF management. Emerging trends, particularly the use of precision medicine, promise to tailor treatments to individual patient profiles, enhancing the efficacy of interventions.